Author
Elizabeth (Izzy) Montgomery, MPA
Policy Analyst
Contact
ACHI Communications
501-526-2244
jlyon@achi.net
With the COVID-19 public health emergency expiring May 11, important changes are on the horizon for COVID-19 testing, treatment, and vaccination coverage. In a previous post, we discussed what the end of the public health emergency would mean for telehealth; in this post, we look at changes individuals and families with different sources of health coverage will experience in access to the tools to fight COVID-19.
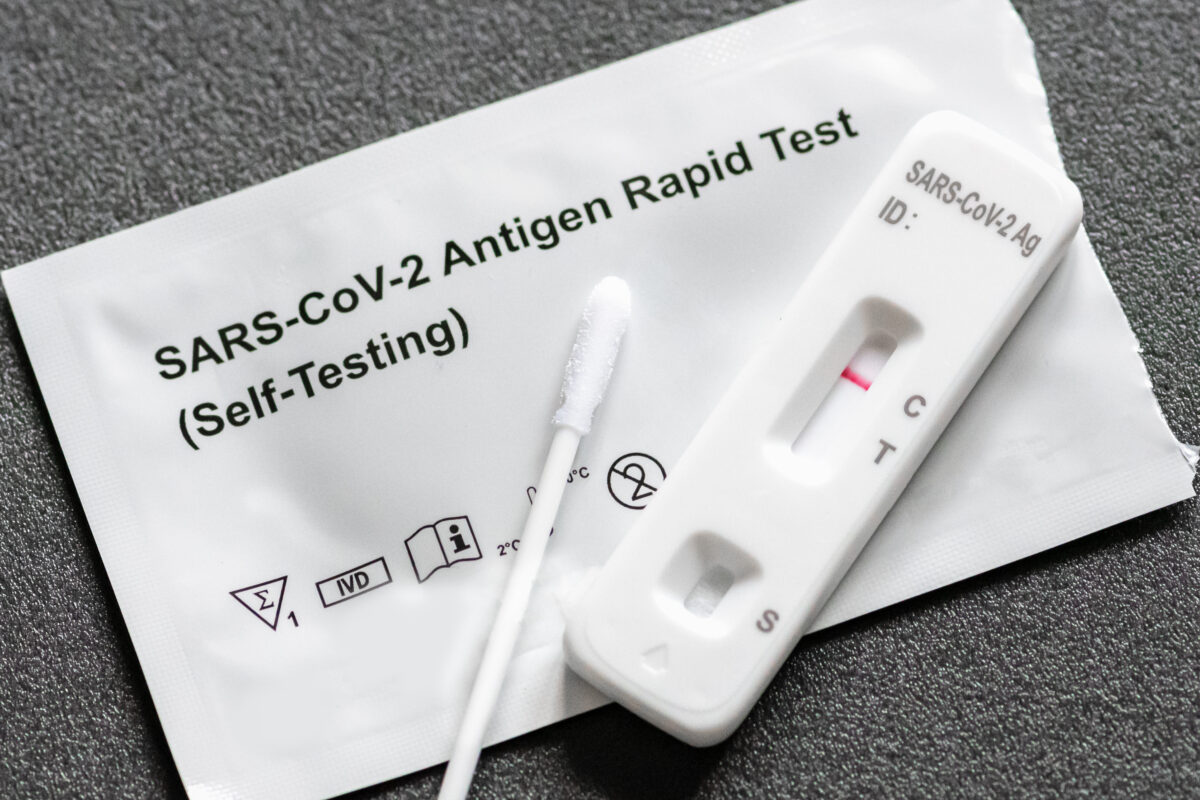
Testing
The Biden administration issued rules in early 2022 requiring insurance companies and group health plans to cover the cost of up to eight at-home COVID-19 tests per month. Clinical diagnostic testing by healthcare providers was also covered for most Americans during the public health emergency. However, changes in the coverage of both at-home and clinical diagnostic tests will vary depending on an individual’s source of coverage once the emergency expires.
- Medicare enrollees in traditional Medicare will be responsible for the full cost of at-home tests when the public health emergency ends. However, coverage for testing at a doctor’s office, pharmacy, or clinic will continue under Medicare Part B coverage (outpatient services) with no individual cost-sharing requirements. Cost-sharing for testing for those enrolled in Medicare Advantage plans may change when the emergency ends, depending on the individual plan.
- Medicaid and Children’s Health Insurance Plan (CHIP) enrollees will have COVID-19 tests and testing-related services covered without cost-sharing through Sept. 30, 2024. After this date, states could limit the number of covered tests or impose some level of cost-sharing.
- Privately insured individuals and families may be subject to cost-sharing requirements for both at-home and clinical diagnostic tests once the PHE expires.
- Individuals who are uninsured will be responsible for at-home and clinical diagnostic test costs once the federal supply of tests is exhausted unless they can acquire free or reduced-cost tests from safety net providers or local nonprofit organizations.
Treatments
The federal government purchased certain Federal Drug Administration (FDA)-approved COVID-19 treatments for no-cost distribution to the public, including the oral antiviral Paxlovid. When the public health emergency ends, coverage for COVID-19 treatments will also vary based on insurance coverage.
- Medicare enrollees will continue to have coverage for COVID-19 treatments when the public health emergency ends, including coverage for the oral antivirals Paxlovid and Lagevrio. Enrollees have faced cost-sharing requirements for hospitalizations or outpatient services (including physician visits and emergency transportation) related to the treatment of COVID-19, but oral antivirals and previously FDA-approved monoclonal antibody treatments did not require cost-sharing. In cases where cost-sharing is already a requirement for treatments, those will continue to apply, according to the Centers for Medicare and Medicaid Services.
- Medicaid and CHIP enrollees will have extended coverage of all FDA-approved drugs and biological products related to COVID-19 treatment through Sept. 30, 2024. Once this period ends, they may be subject to cost-sharing.
- Privately insured individuals and families were never guaranteed coverage for COVID-19 treatments under federal law. As government supply dwindles, those with private insurance could face cost-sharing requirements or premium increases related to COVID-19 treatment.
- Individuals who are uninsured will also be impacted when the federal government’s supply of COVID-19 treatments is exhausted and will face out-of-pocket costs to obtain drugs like Paxlovid.
Vaccines
The federal government has purchased and distributed COVID-19 vaccines since they first began receiving emergency authorization in late 2020, allowing most Americans to receive these vaccines at no cost. As the public health emergency ends and government-purchased supplies are exhausted, vaccine manufacturers have signaled they will raise the prices of vaccines. However, many Americans will continue to have access to COVID-19 vaccines without cost-sharing, as summarized below.
- Medicare enrollees will still have access to COVID-19 vaccines at no out-of-pocket cost through Medicare Part B (outpatient medical coverage) after the end of the public health emergency.
- Medicaid and CHIP enrollees will also have access to COVID-19 vaccines once the public health emergency ends at no out-of-pocket cost. Provisions in the American Rescue Act and the Inflation Reduction Act mandate that Medicaid programs cover all vaccines recommended by the Advisory Committee on Immunization Practices with no cost-sharing requirements for beneficiaries.
- Most individuals and families with private insurance will continue having access to vaccines at no out-of-pocket cost, but there are some exceptions. These include grandfathered plans under the Affordable Care Act and short-term, limited-duration plans, which are not subject to the healthcare law’s preventive services coverage requirement. Individuals on these plans may be responsible for all or part of their COVID-19 vaccines in the future.
- The uninsured may be responsible for the full cost of the vaccine, or they may be able to obtain low-cost or free vaccines from community clinics or other healthcare providers. With COVID-19 vaccine prices rising, there are concerns that the uninsured may forgo vaccination with the end of the public health emergency. However, one COVID-19 vaccine manufacturer, Modera, has pledged to offer free vaccines for the uninsured or underinsured once the public health emergency ends.