Maternal and Infant Health
Arkansas has one of the highest maternal mortality rates in the nation, making it one of the riskiest places to have a baby. Our state also has the third-highest infant mortality rate, behind only Louisiana and Mississippi. This page highlights key statistics and other information about maternal and infant health in Arkansas. It is intended to raise awareness, promote discussion, and inform policymakers and stakeholders as they engage with this issue to make our state a healthier place for mothers and infants.
Featured
Birthing Journey
Reports and Explainers
Arkansas Birthing Hospitals
Interviews
Blog Posts
Podcast Episodes
News Releases
Acute Behavioral Health Events Along the Birthing Journey in Arkansas
Behavioral health events, including mental health and substance abuse diagnoses, in the prenatal and postpartum periods impact mothers and their families during a critical time in their lives. As part of our continuing effort to examine each step along the birthing journey in Arkansas, ACHI developed an interactive dashboard to allow policymakers, healthcare providers, and community leaders to research acute behavioral health events among Arkansas mothers at the state, regional, and county levels.
The dashboard below displays data on acute behavioral health events — those that result in an emergency department (ED) visit or inpatient stay — in the prenatal and postpartum periods among 80,704 Arkansas mothers who gave birth between Jan. 1, 2019, and June 30, 2022.
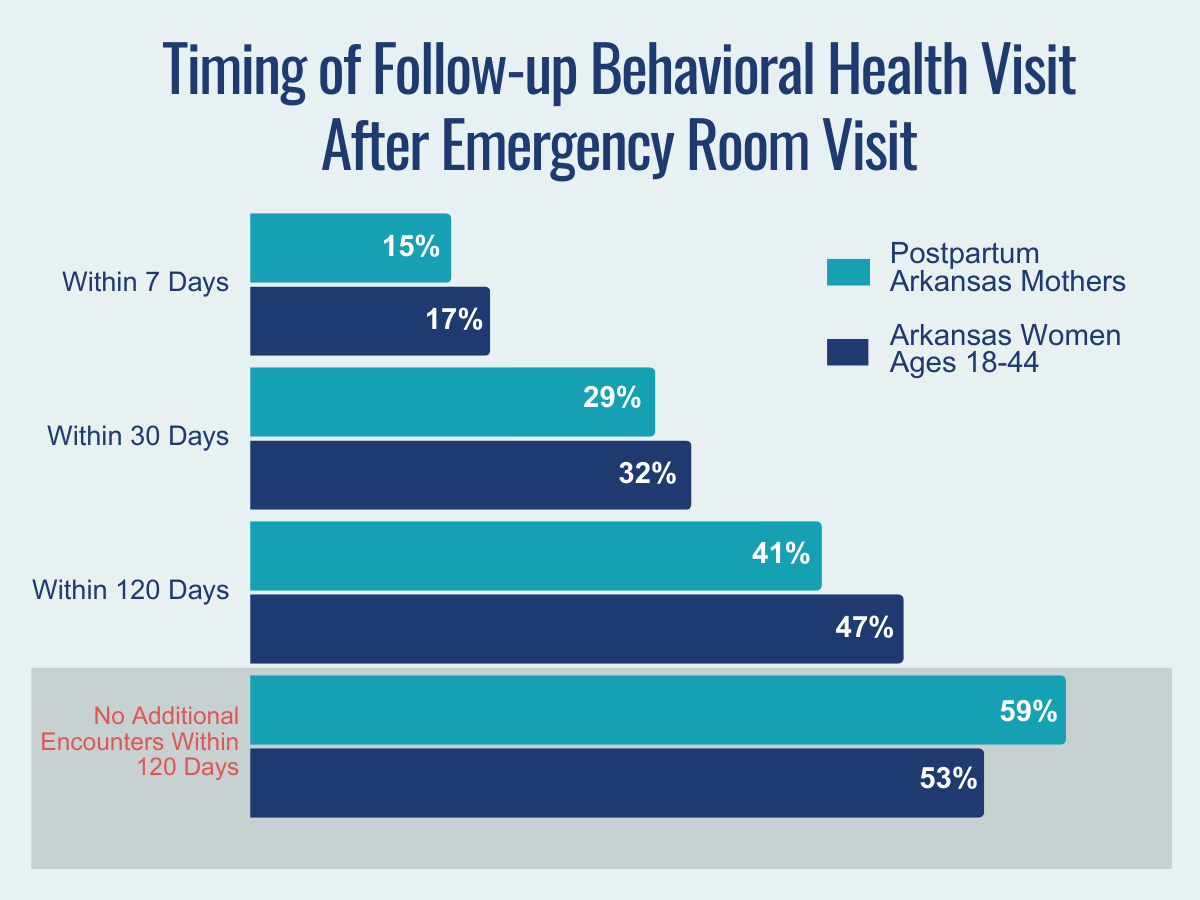
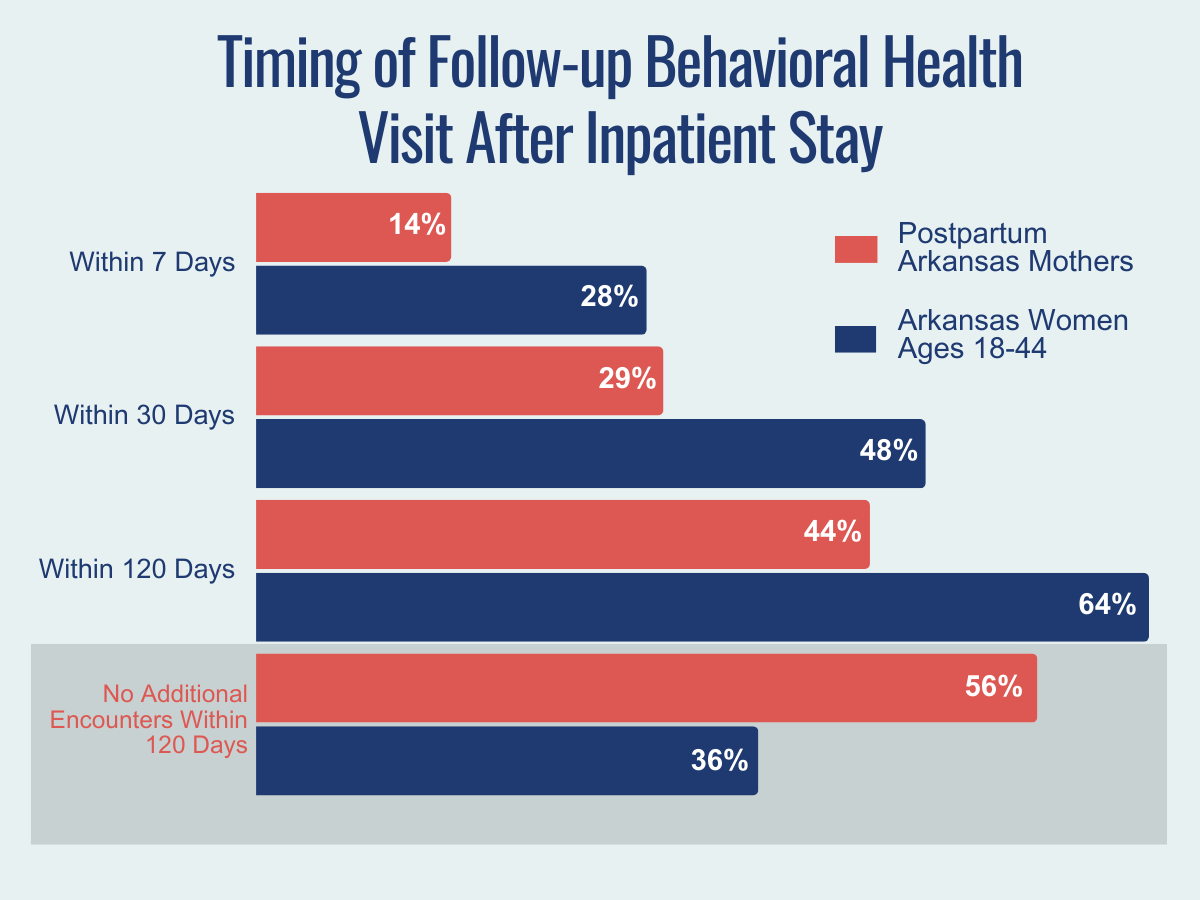
ACHI’s analysis of these data included an examination of the timing of postpartum mothers’ follow-up visits within 120 days of either an emergency room visit or inpatient stay for a behavioral health event. Key findings from ACHI’s analysis are displayed in our maternal behavioral health infographic. They include:
- Behavioral health events were more likely to occur in the postpartum period compared to the prenatal period.
- Postpartum mothers consistently had lower follow-up visit rates after an emergency department visit or an inpatient stay compared to all women ages 18-44 in Arkansas.
- 59% of postpartum mothers had no outpatient follow-up behavioral health visit within 120 days of an emergency department visit.
- 56% of postpartum mothers had no outpatient follow-up behavioral health visit within 120 days of an inpatient stay.
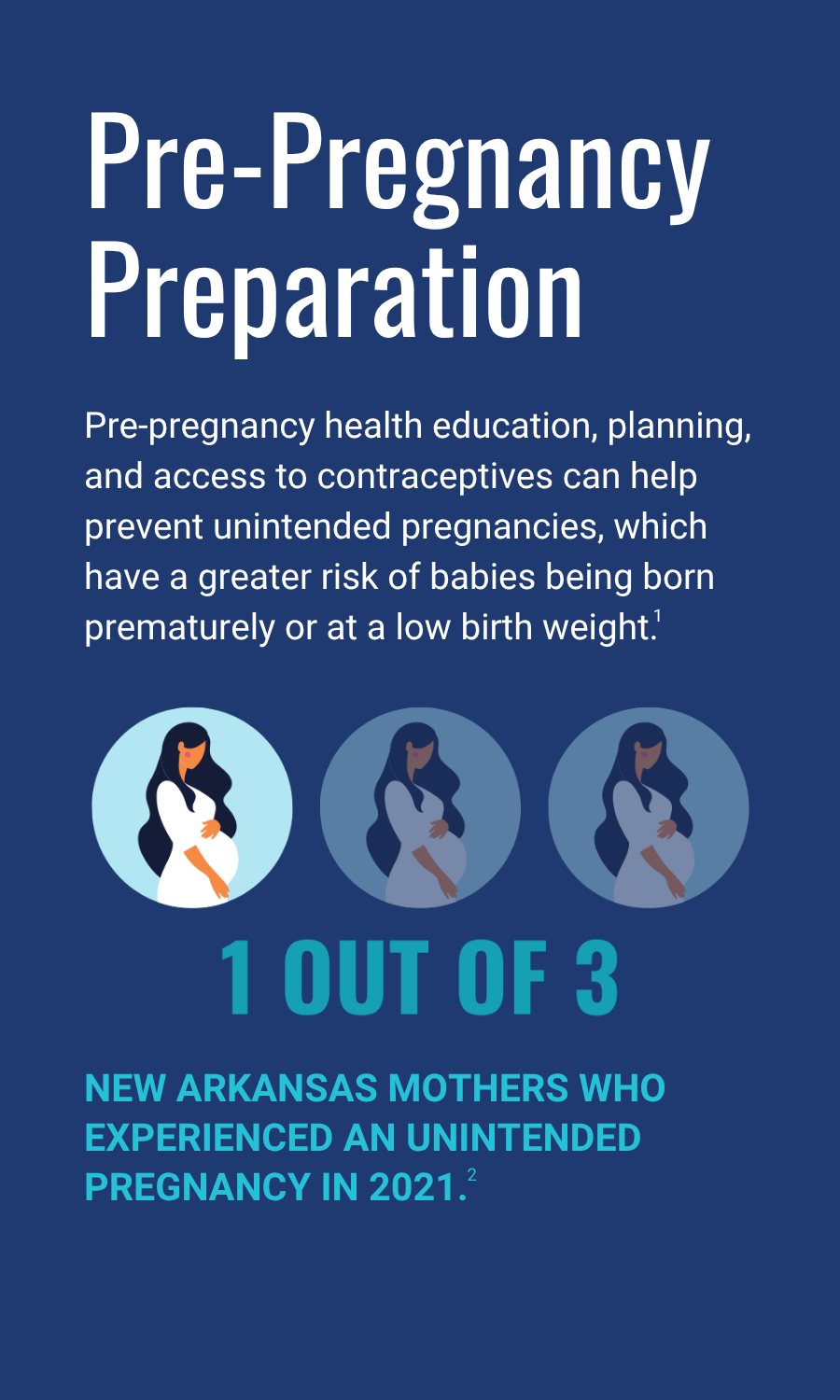
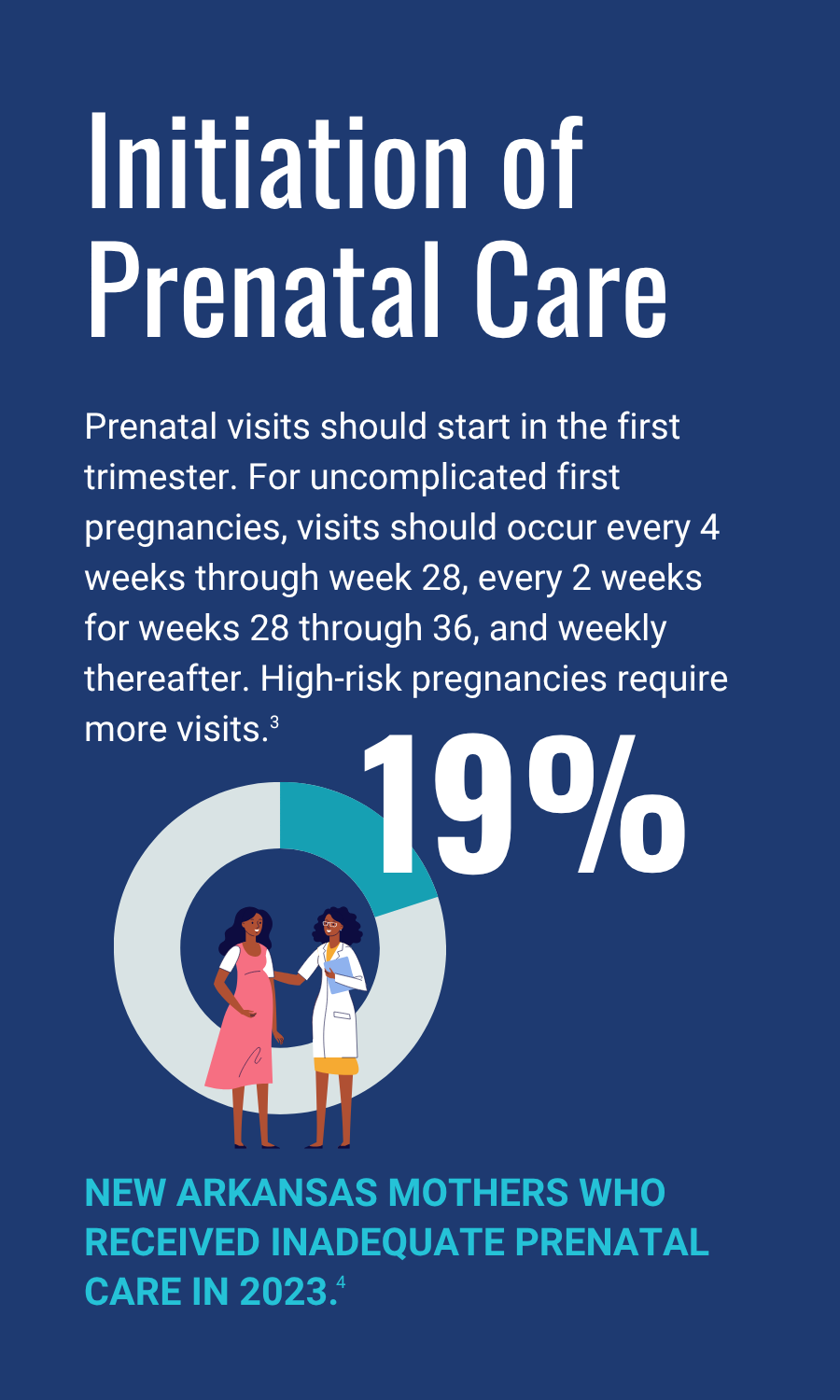
9 POINTS ON A HEALTHY BIRTHING JOURNEY
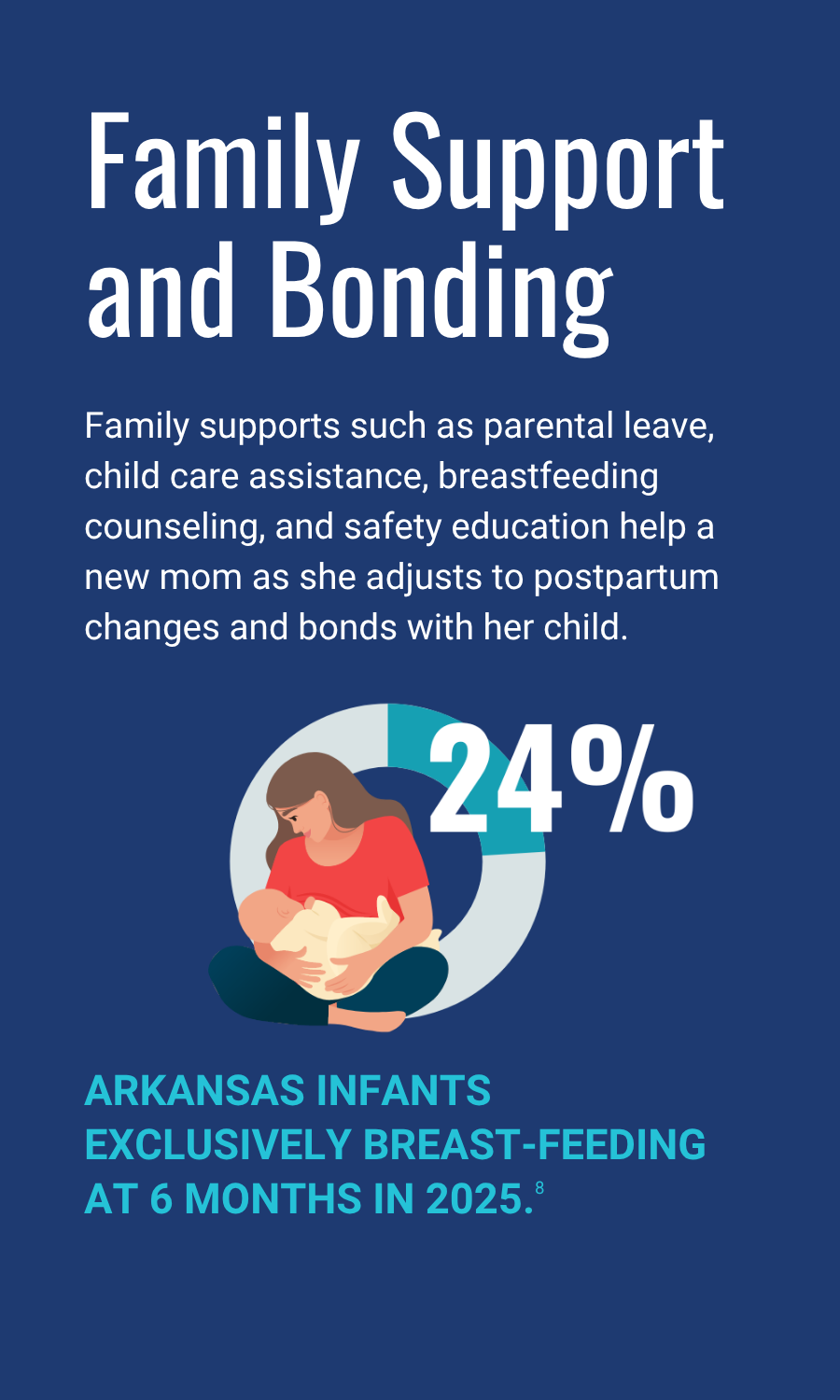
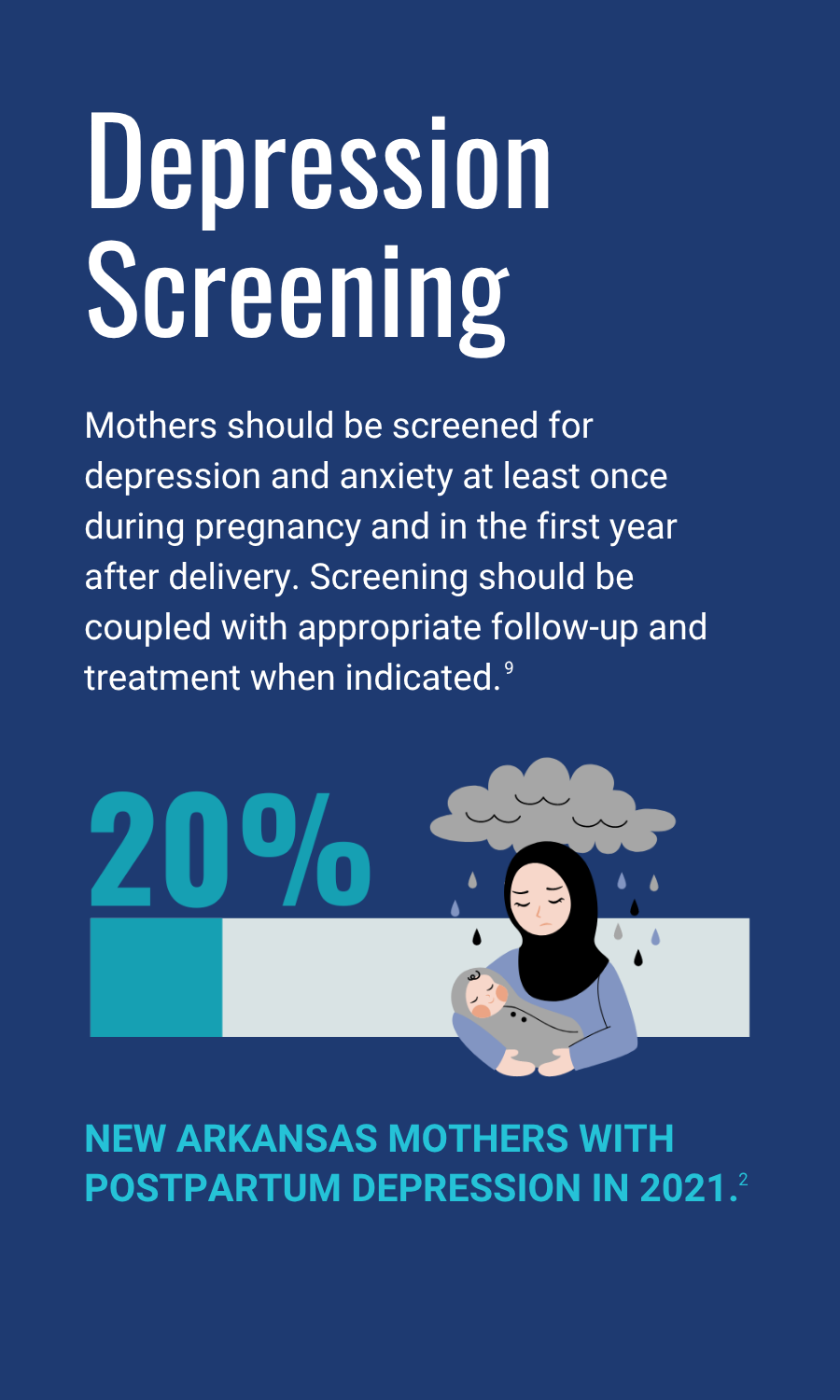
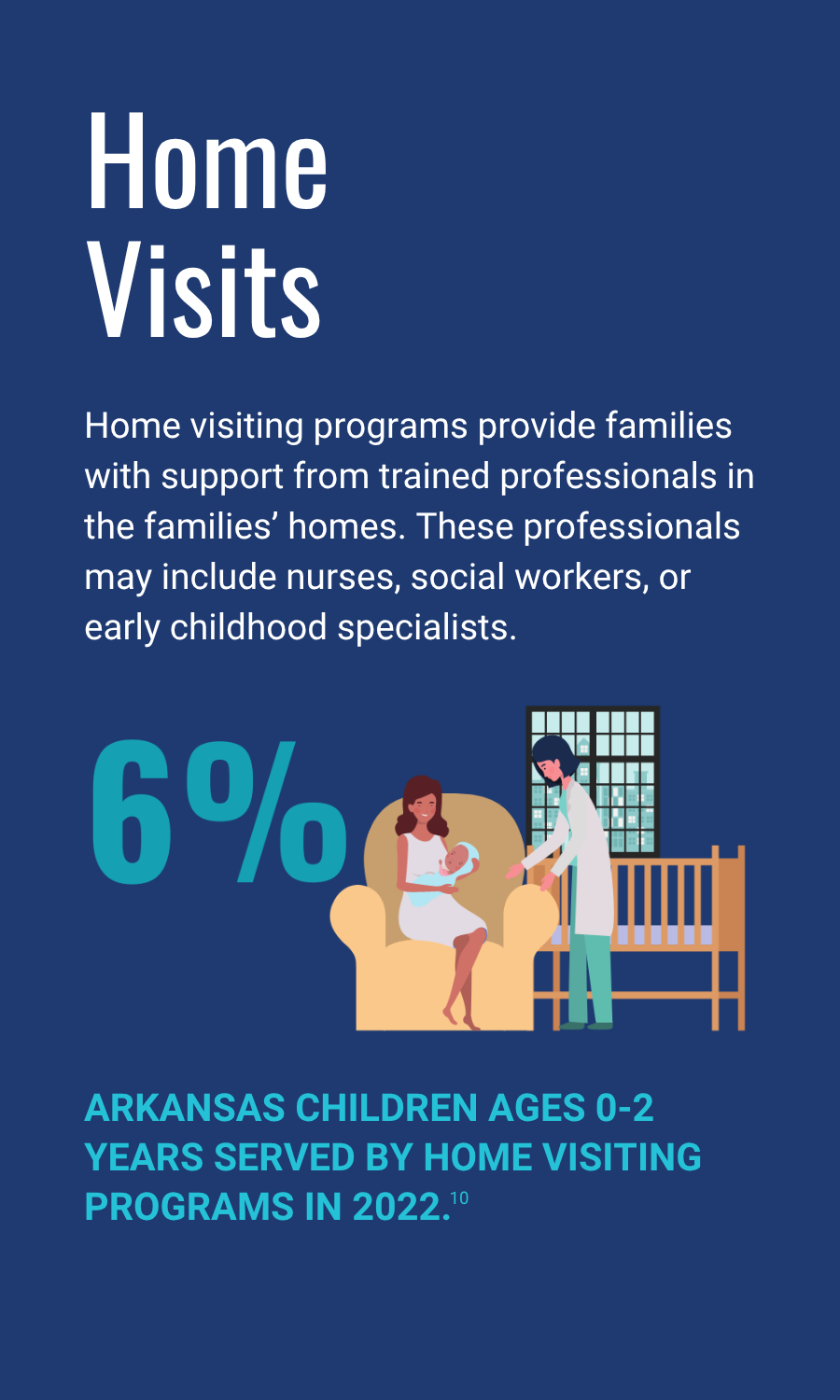
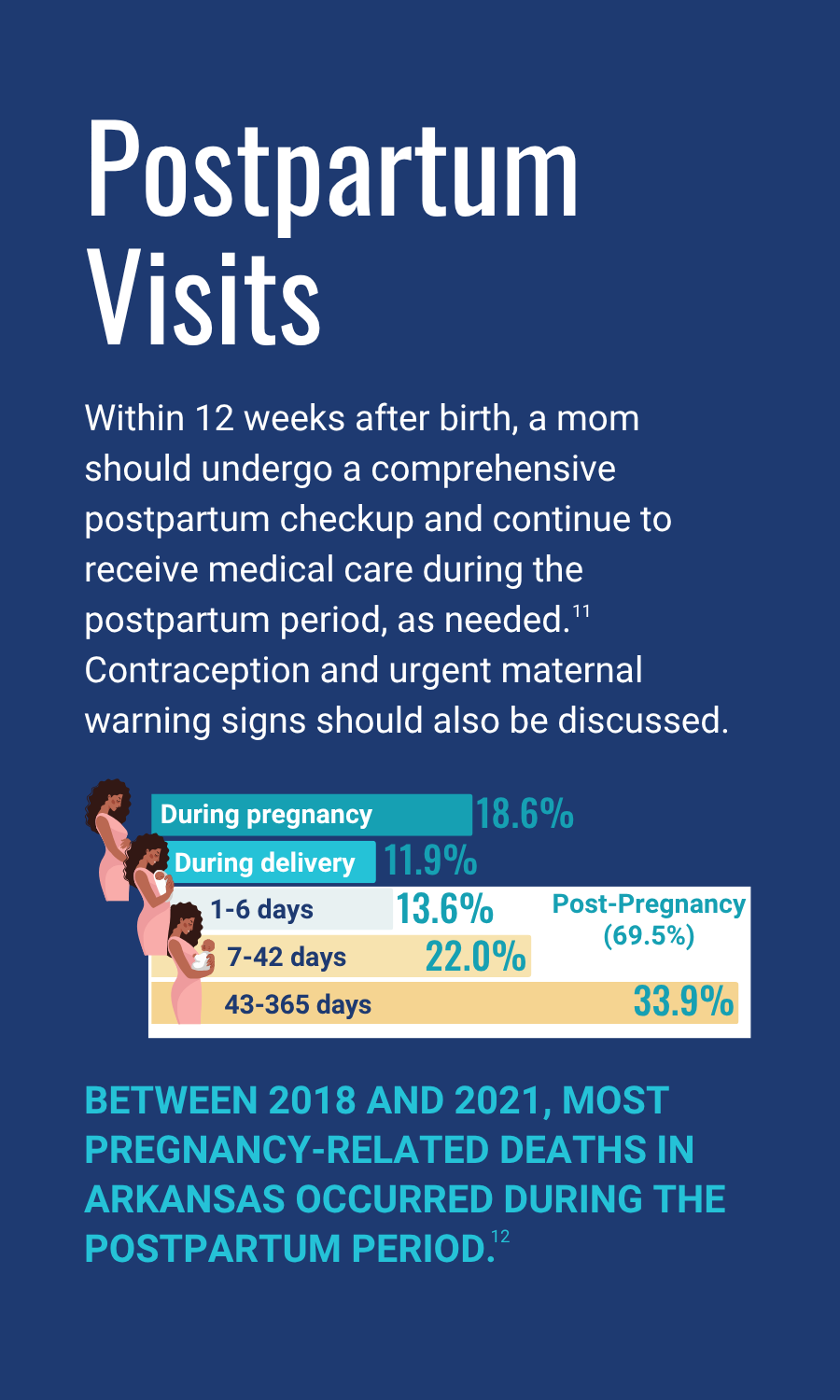
In an effort to raise awareness about Arkansas’s maternal and infant health challenges and suggest policy solutions, ACHI created an infographic depicting what a birthing journey for new mothers should be in order to achieve better maternal and infant health outcomes.
Severe Maternal Morbidity in Arkansas
As part of ACHI’s continuing effort to examine each step of the birthing journey in Arkansas, we developed an infographic highlighting the impact of severe maternal morbidity (SMM), defined by the Centers for Disease Control and Prevention as “unexpected outcomes of labor and delivery that result in significant short- or long-term health consequences.” Examples include sepsis, acute renal failure, and acute heart failure.
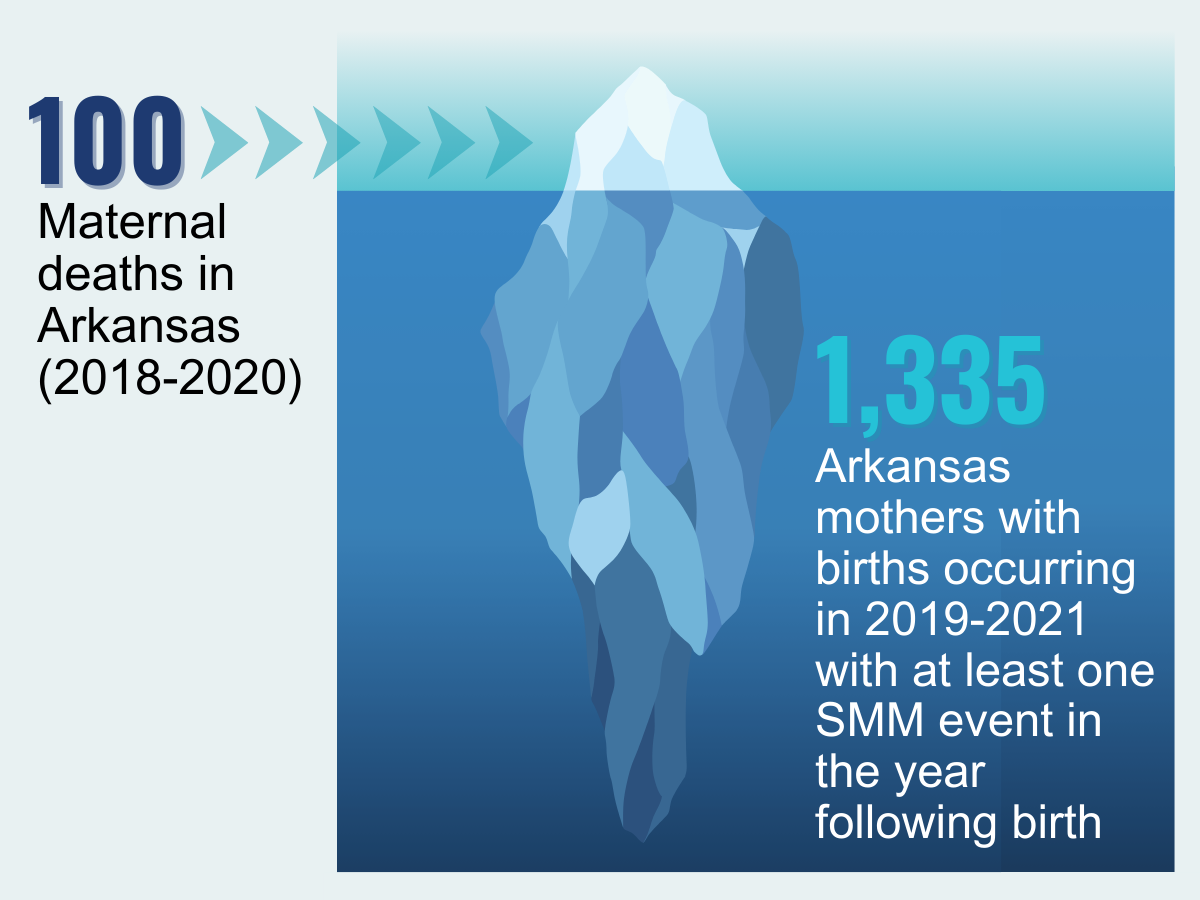
Maternal mortality has been described as the “tip of the iceberg” and severe maternal morbidity as the base. SMM events, also known as maternal near-miss events, occur much more frequently than maternal deaths despite receiving less public attention.
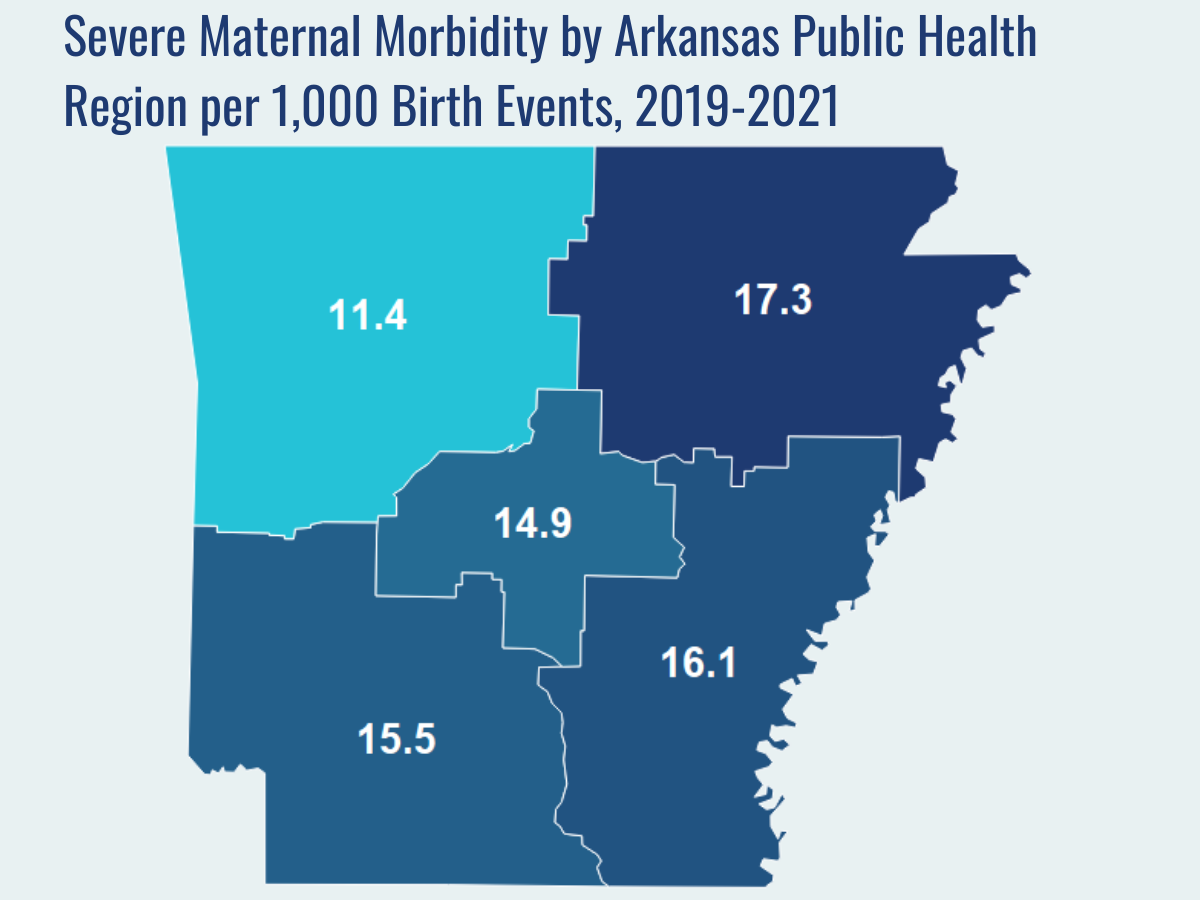
ACHI analyzed hospital discharge data for births that occurred between 2019 and 2021 to determine the impact of SMM among those mothers up to one year postpartum.
Key findings:
- While 100 maternal deaths occurred in Arkansas between 2018 and 2020, 1,335 mothers with births between 2019 and 2021 experienced at least one SMM event up to a year after birth (comparable maternal deaths and SMM from identical periods were not available due to data limitations, but our analysis will be updated when 2021 maternal death data are available).
- Between 2019 and 2021, for every 1,000 birth events (i.e., hospitalizations during which at least one delivery occurred) in Arkansas, 14.2 were associated with at least one SMM event.
- SMM events most commonly occurred during birth (44.8%), but 34.9% occurred more than six weeks after discharge, 10.6% occurred within a week after discharge, and the remaining 9.7% occurred two to six weeks after discharge.
- The five most common types of SMM were sepsis (3.8 per 1,000 birth events), adult respiratory distress syndrome (3.1 per 1,000 birth events), acute renal failure (2.8 per 1,000 birth events); pulmonary edema/acute heart failure (2 per 1,000 birth events); and hysterectomy (1.9 per 1,000 birth events).
- Geographically, SMM was most common in the Northeast Public Health Region (17.3 per 1,000 birth events) followed by the Southeast Region (16.1 per 1,000 birth events), the Southwest Region (15.5 per 1,000 birth events), the Central Region (14.9 per 1,000 birth events), and the Northwest Region (11.4 per 1,000 birth events).
- By age, SMM was highest among women 40 and older (27.3 per 1,000 birth events), followed by women aged 35-39 (21.9 per 1,000 birth events), women aged 30-34 (14.6 per 1,000 birth events), women aged 25-29 (13.1 per 1,000 birth events), women under 20 (13.2 per 1,000 birth events), and women aged 20-24 (11.3 per 1,000 birth events).
- By race and ethnicity, SMM was highest among Black women (22.2 per 1,000 birth events), followed by women whose race was identified as Other (21.6 per 1,000 birth events), Asian/Pacific Islander women (18.1 per 1,000 birth events), White women (12.5 per 1,000 birth events), Hispanic women (9.6 per 1,000 birth events), and American Indian/Alaskan Native women (6.8 per 1,000 birth events).
Related Reports and Explainers
Who Is Delivering Babies in Northwest Arkansas?
Who Is Delivering Babies in Arkansas?
Long-Acting Reversible Contraception: An Overview
C-Section Rates in Arkansas
100 ARKANSAS MOMS
The health of a mother can play a significant role throughout the birthing journey. As part of ACHI’s 100 Arkansans initiative to illustrate demographic and health statistics, we examined important risk factors among Arkansas moms from pre-pregnancy through postpartum, including recent healthcare visits, access to insurance coverage, body mass index, tobacco use, vaccinations, and other factors.

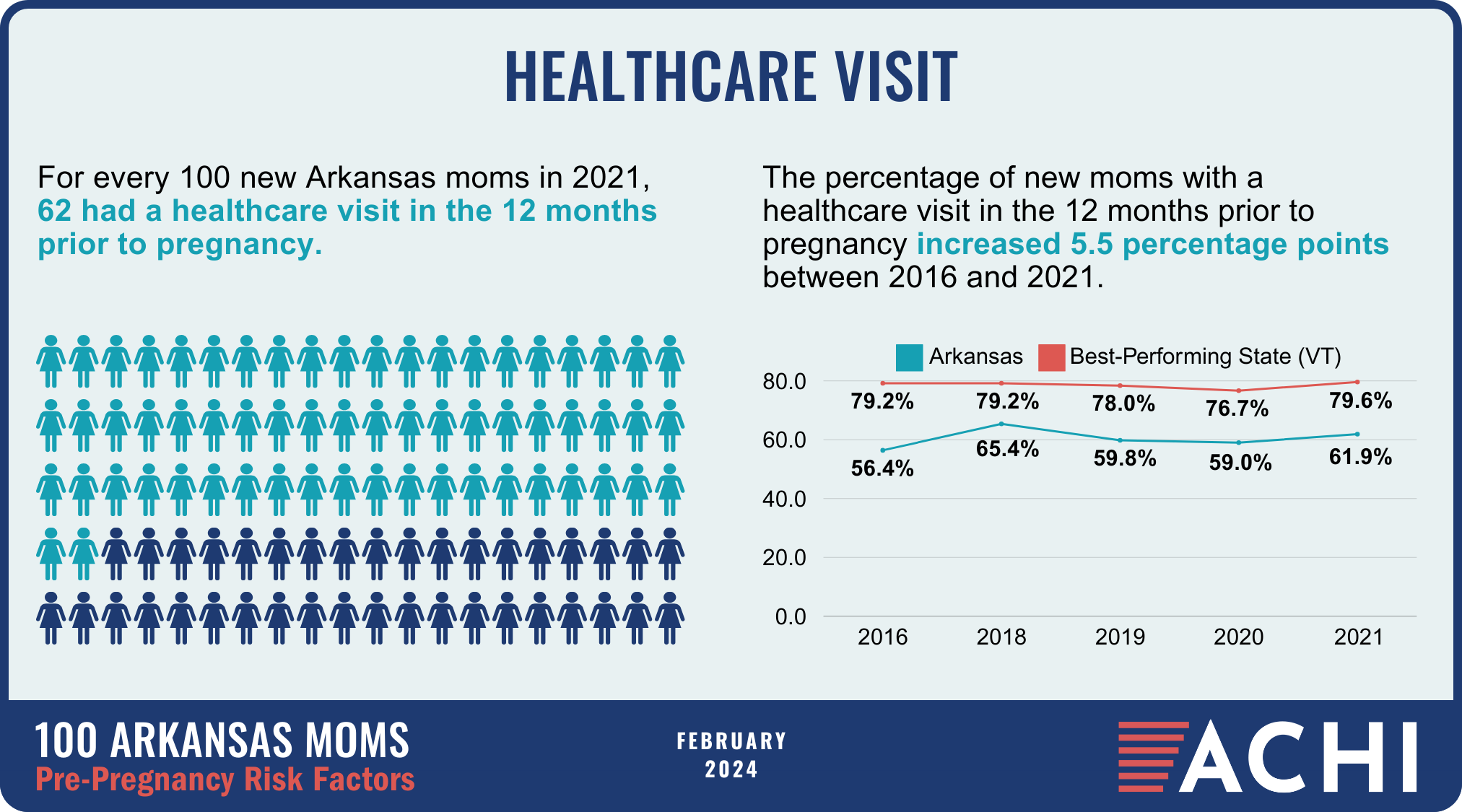
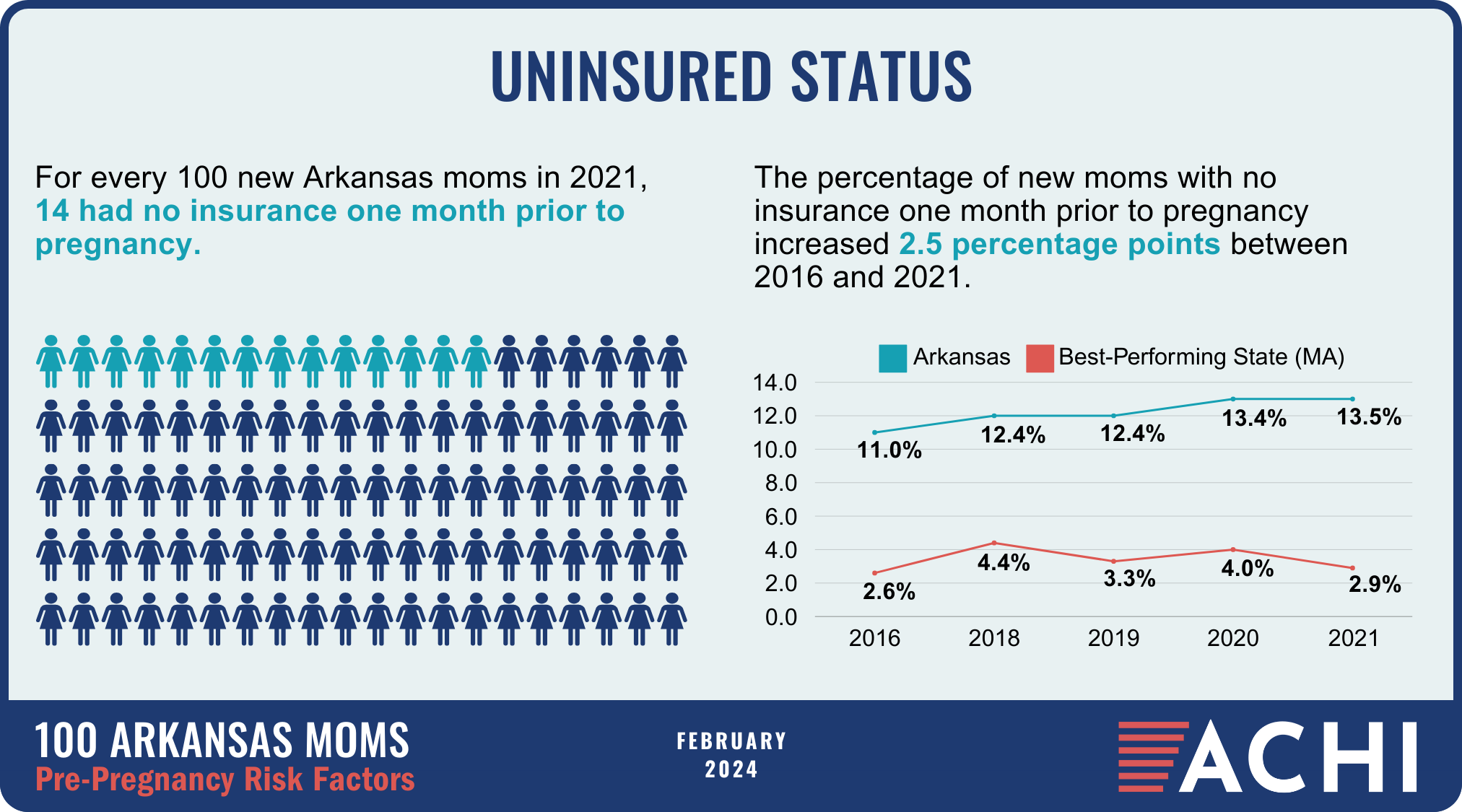
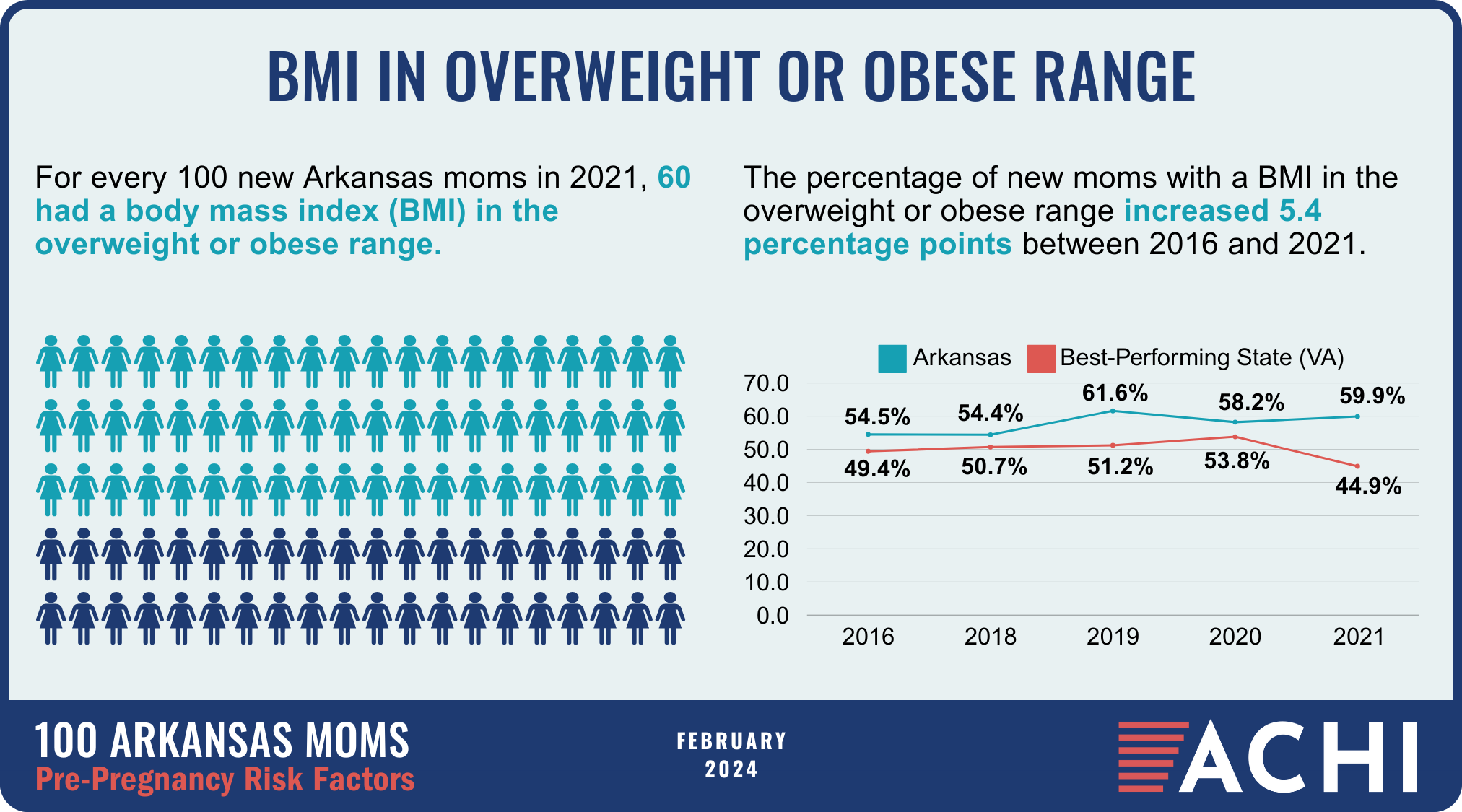
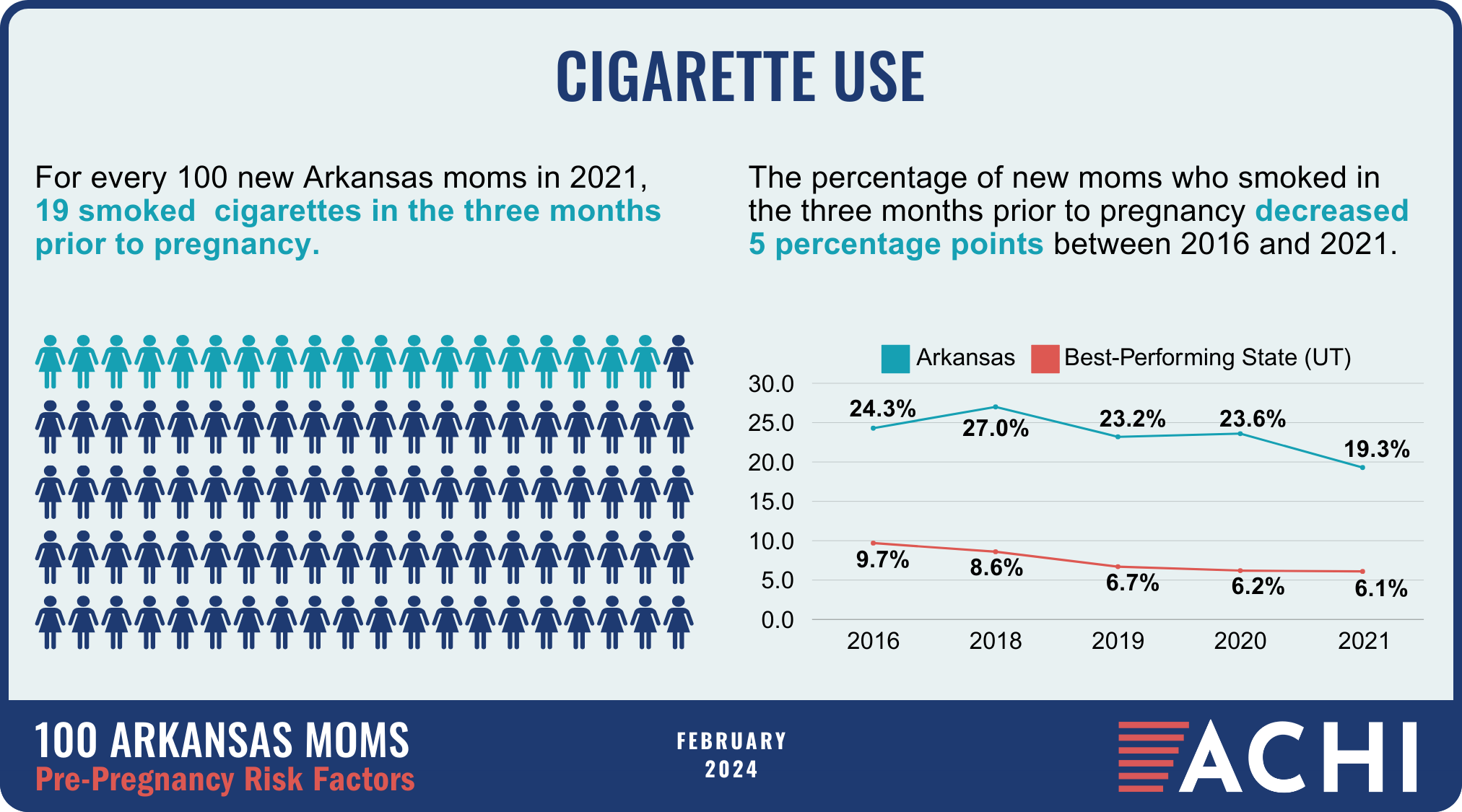
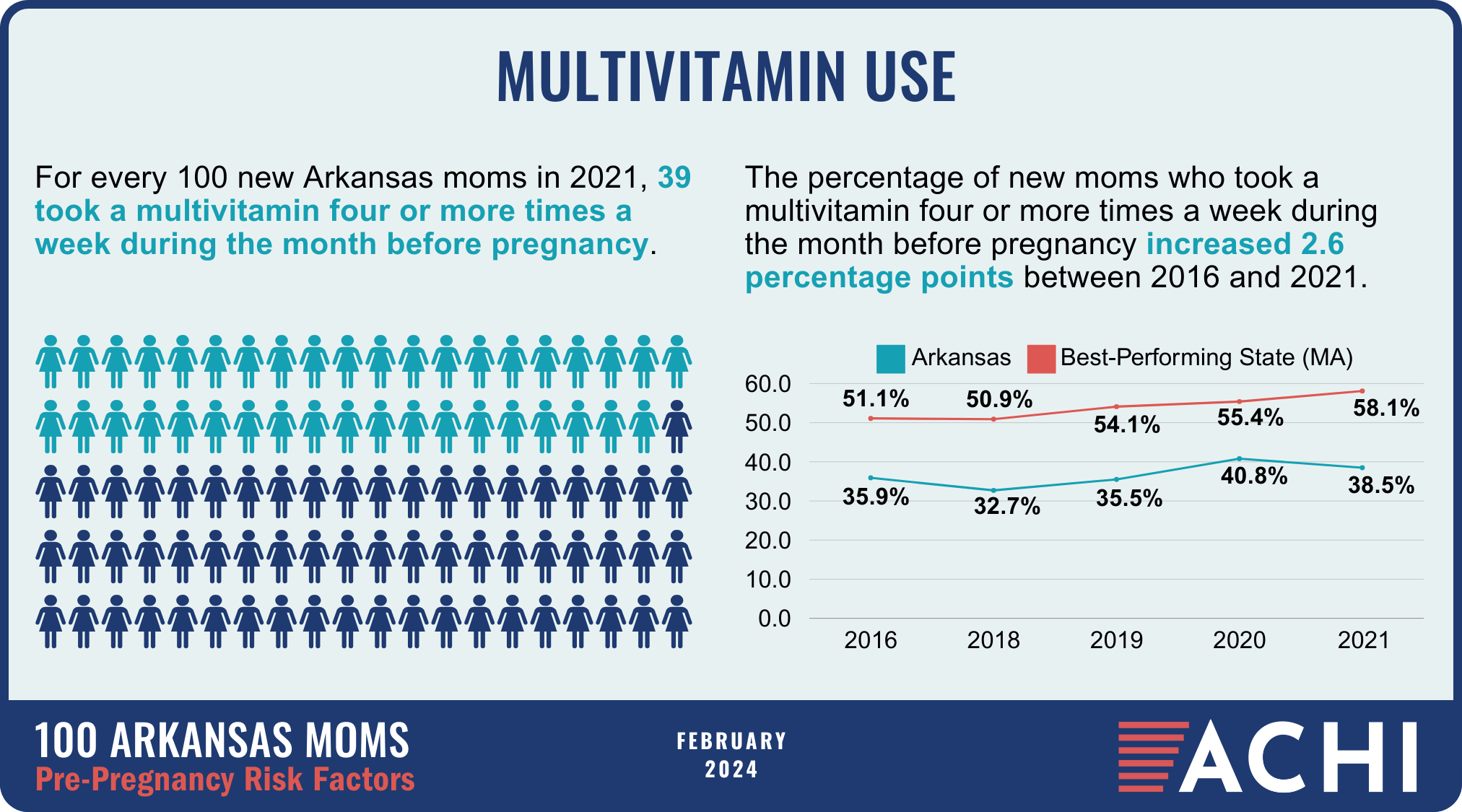
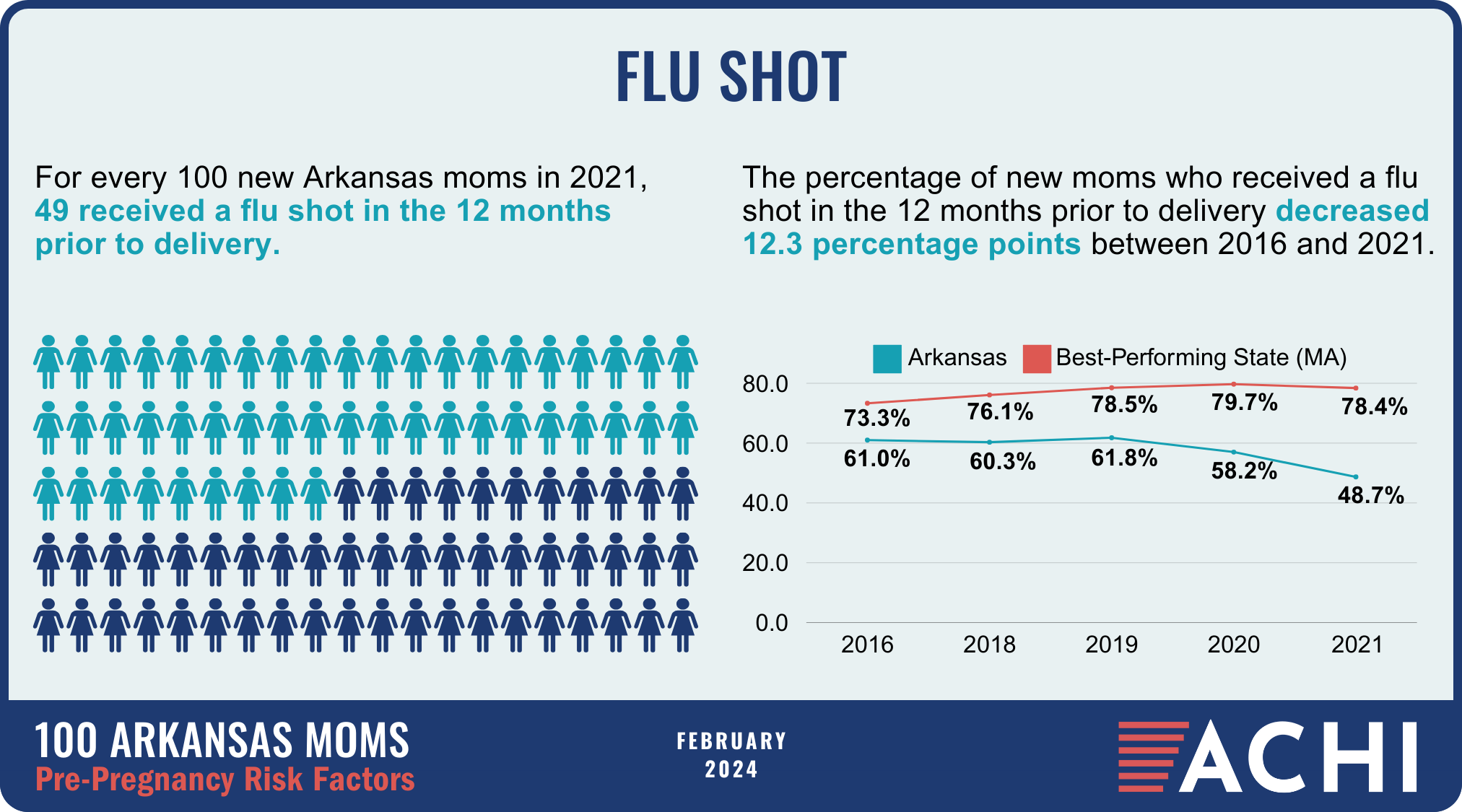
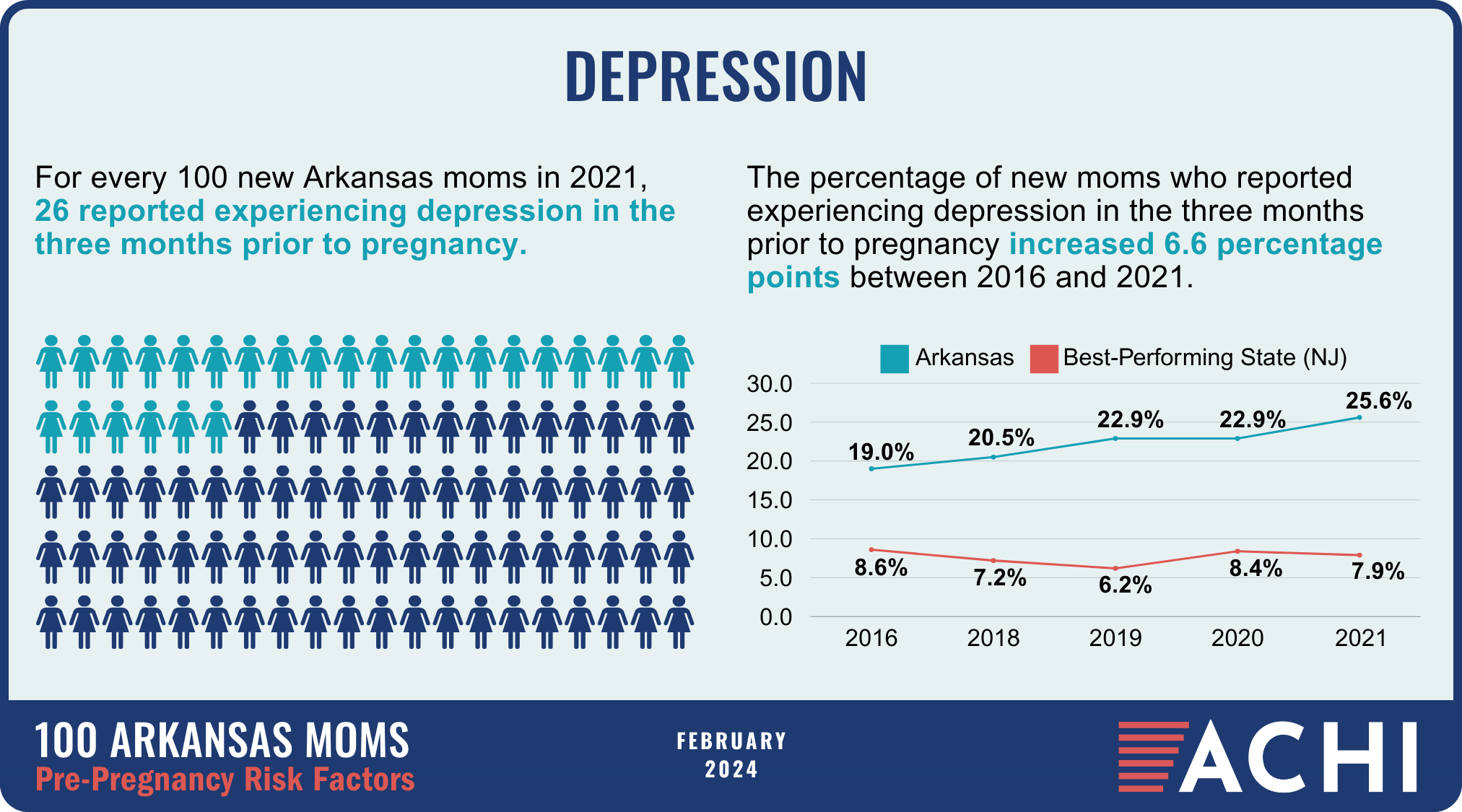
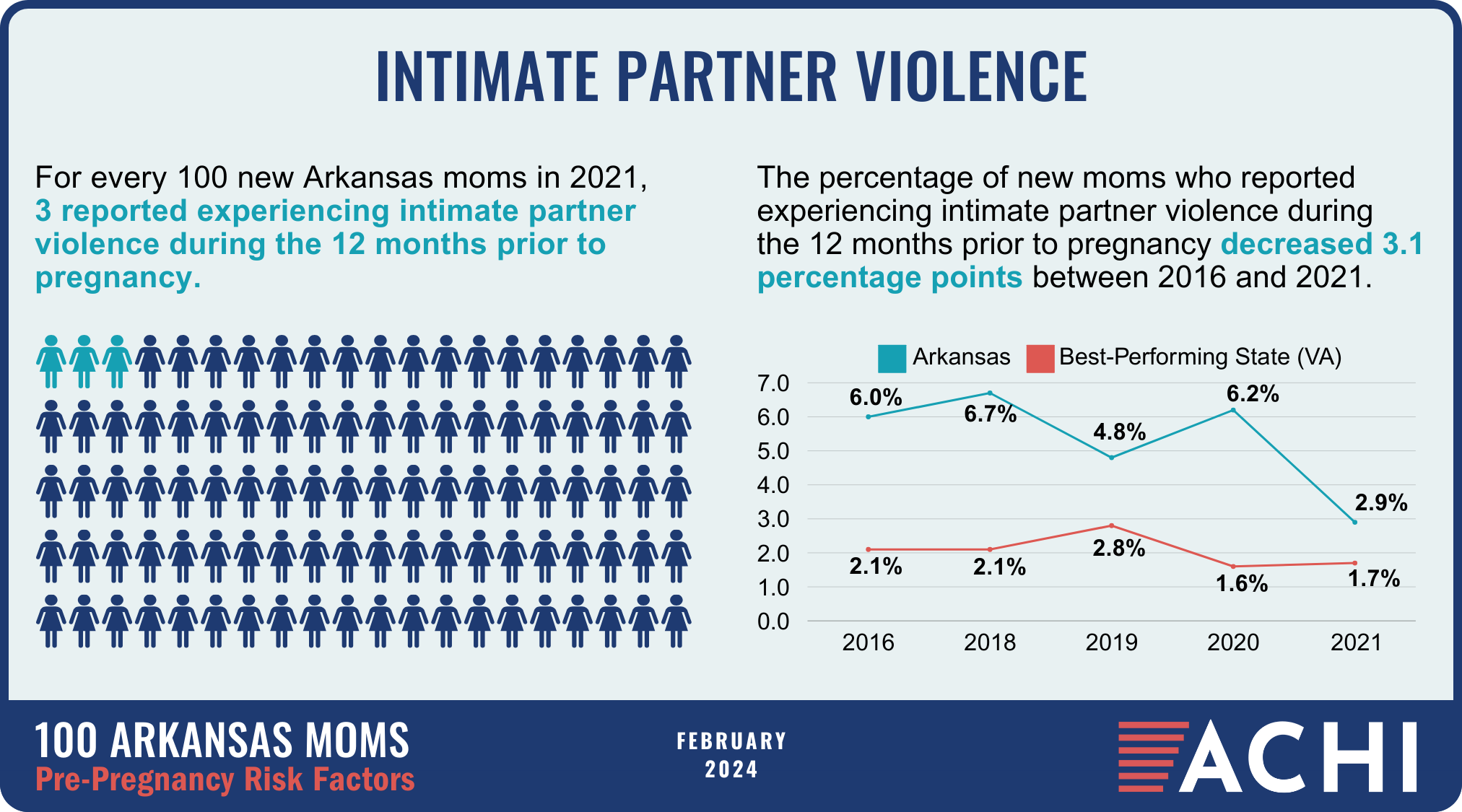
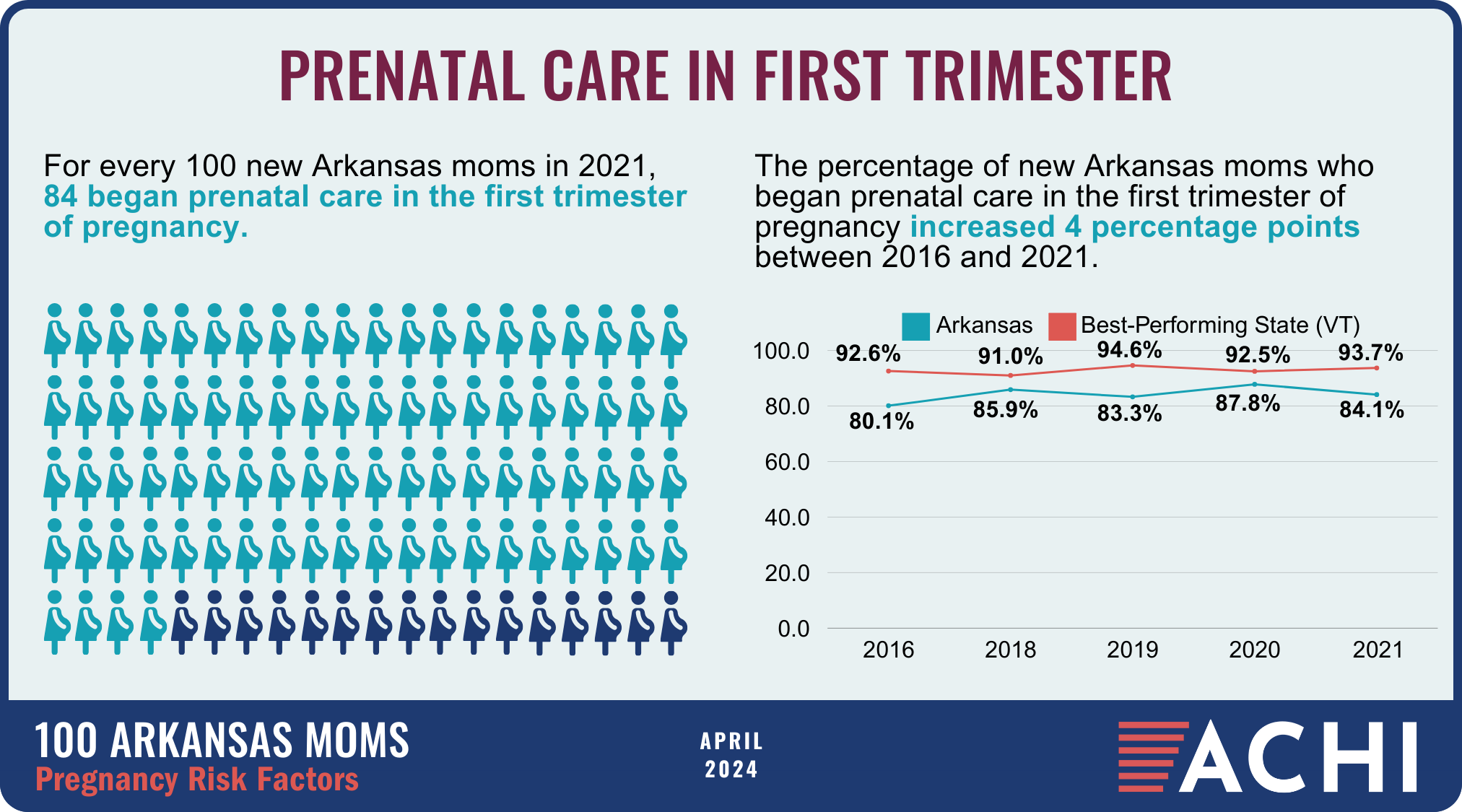
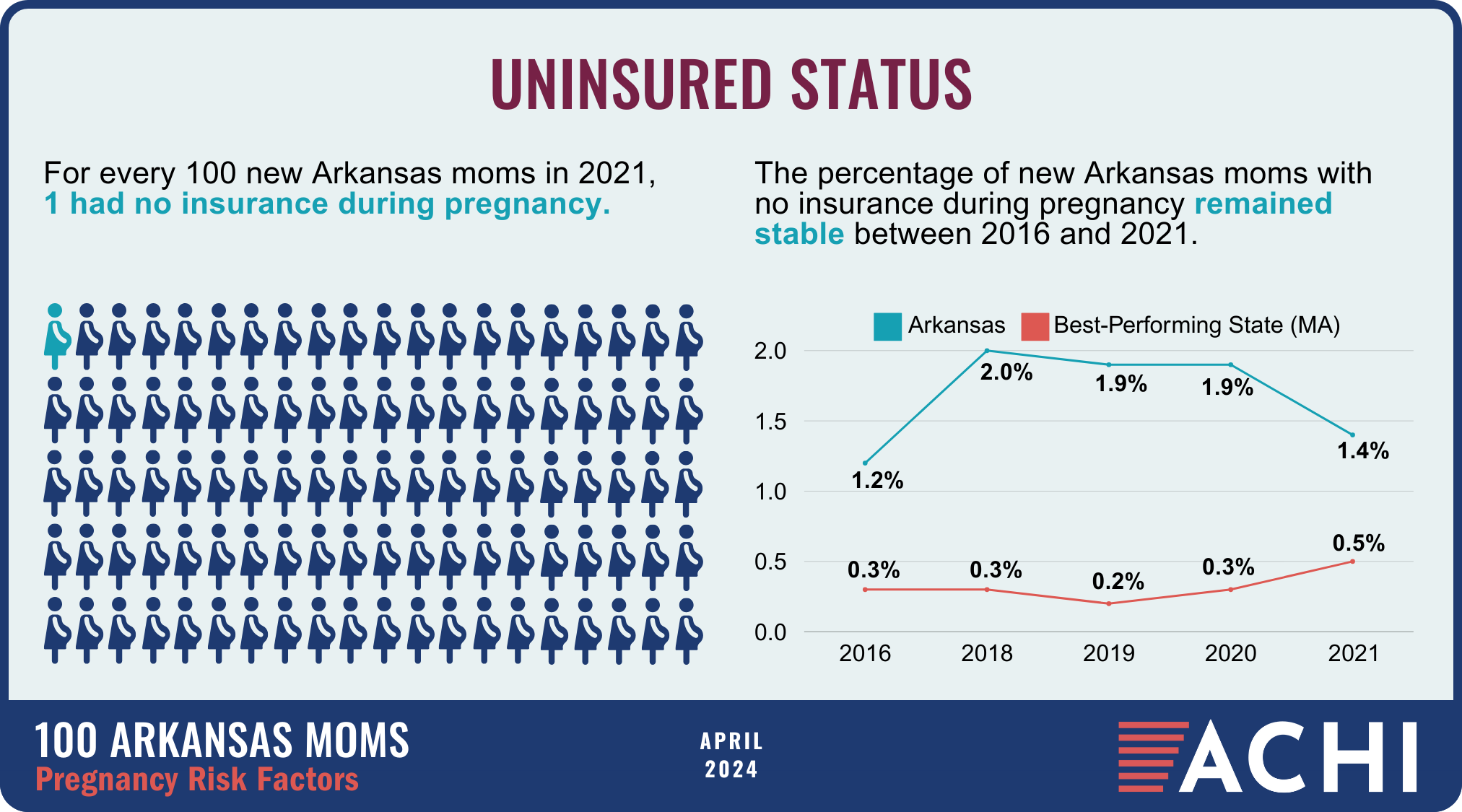
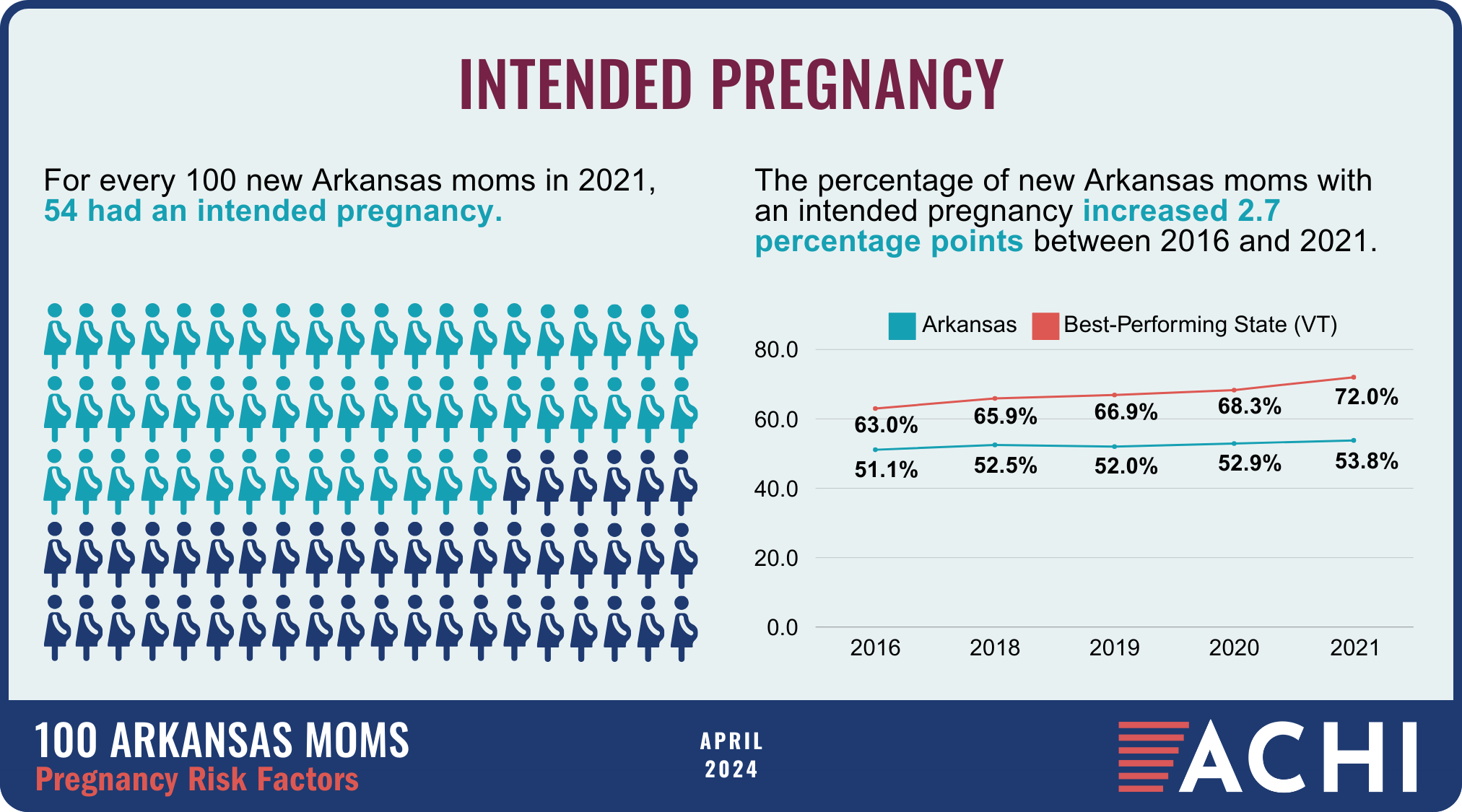
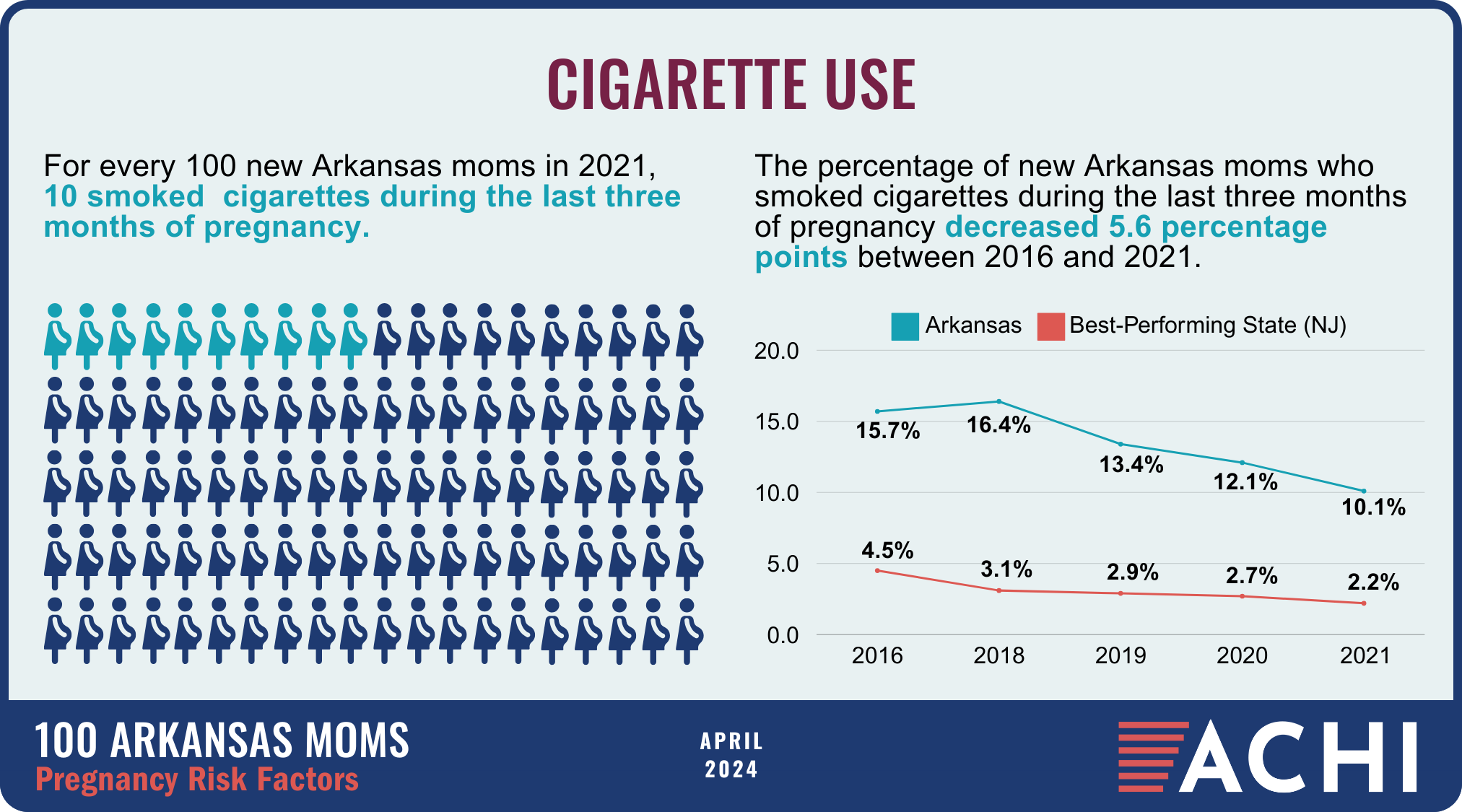
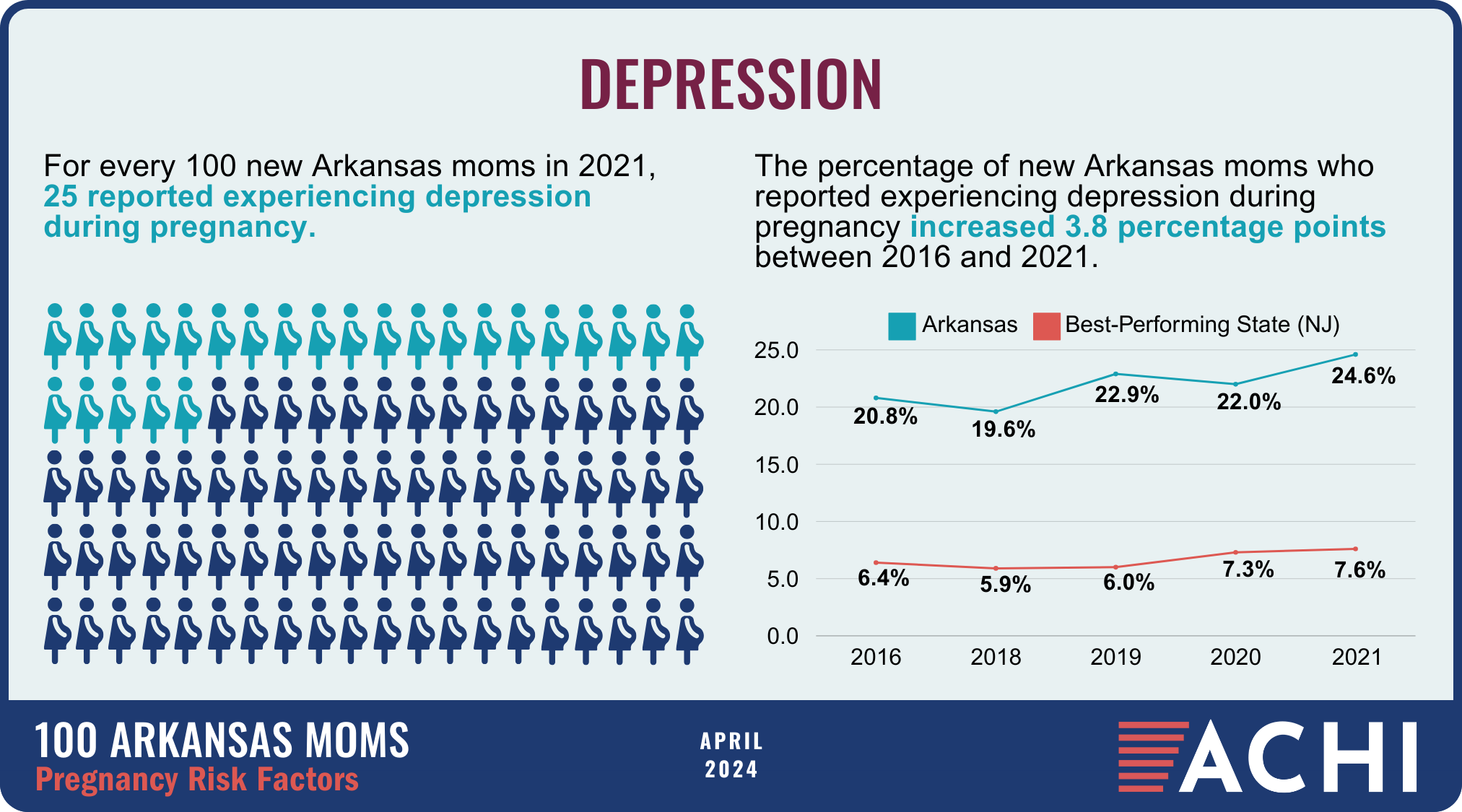
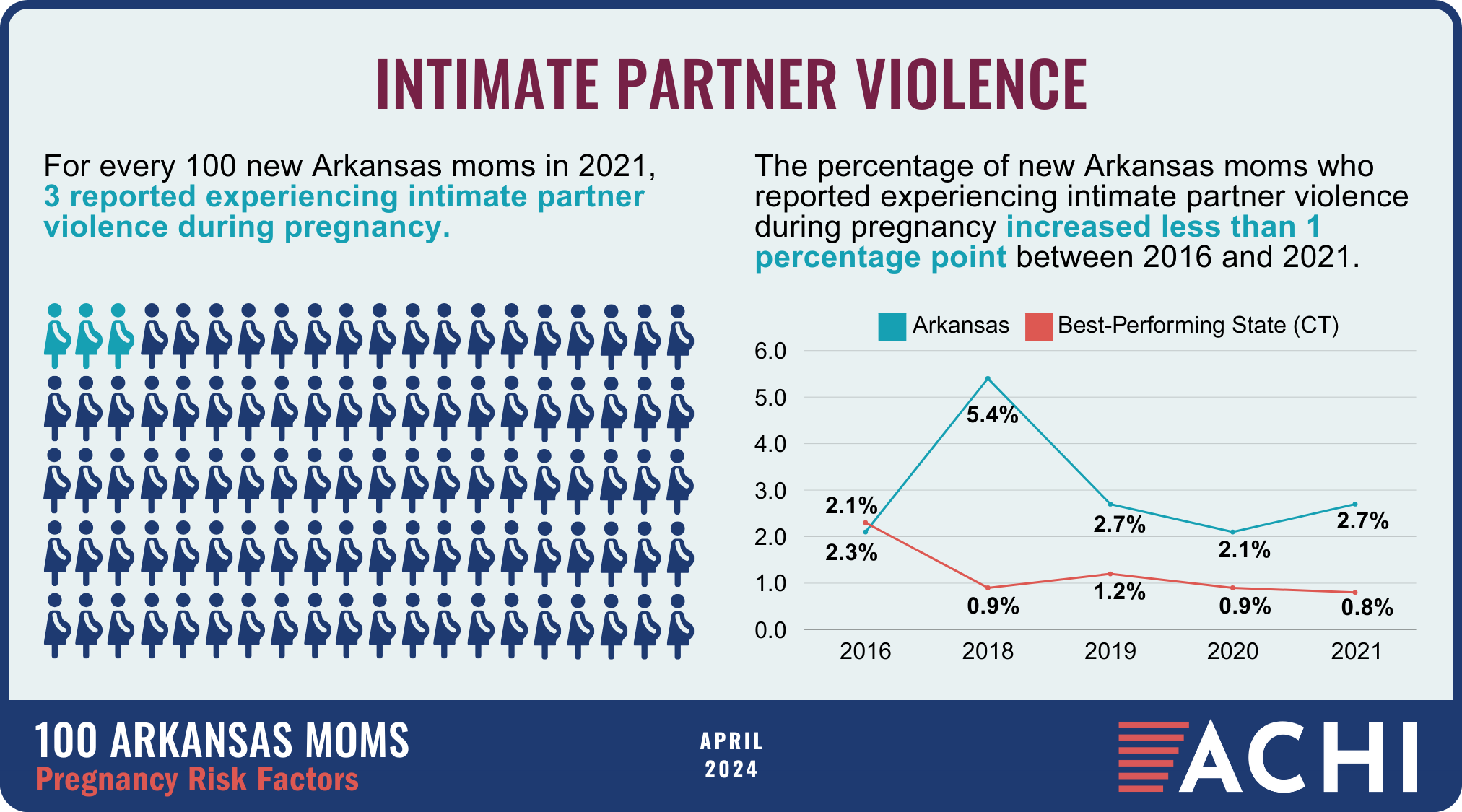
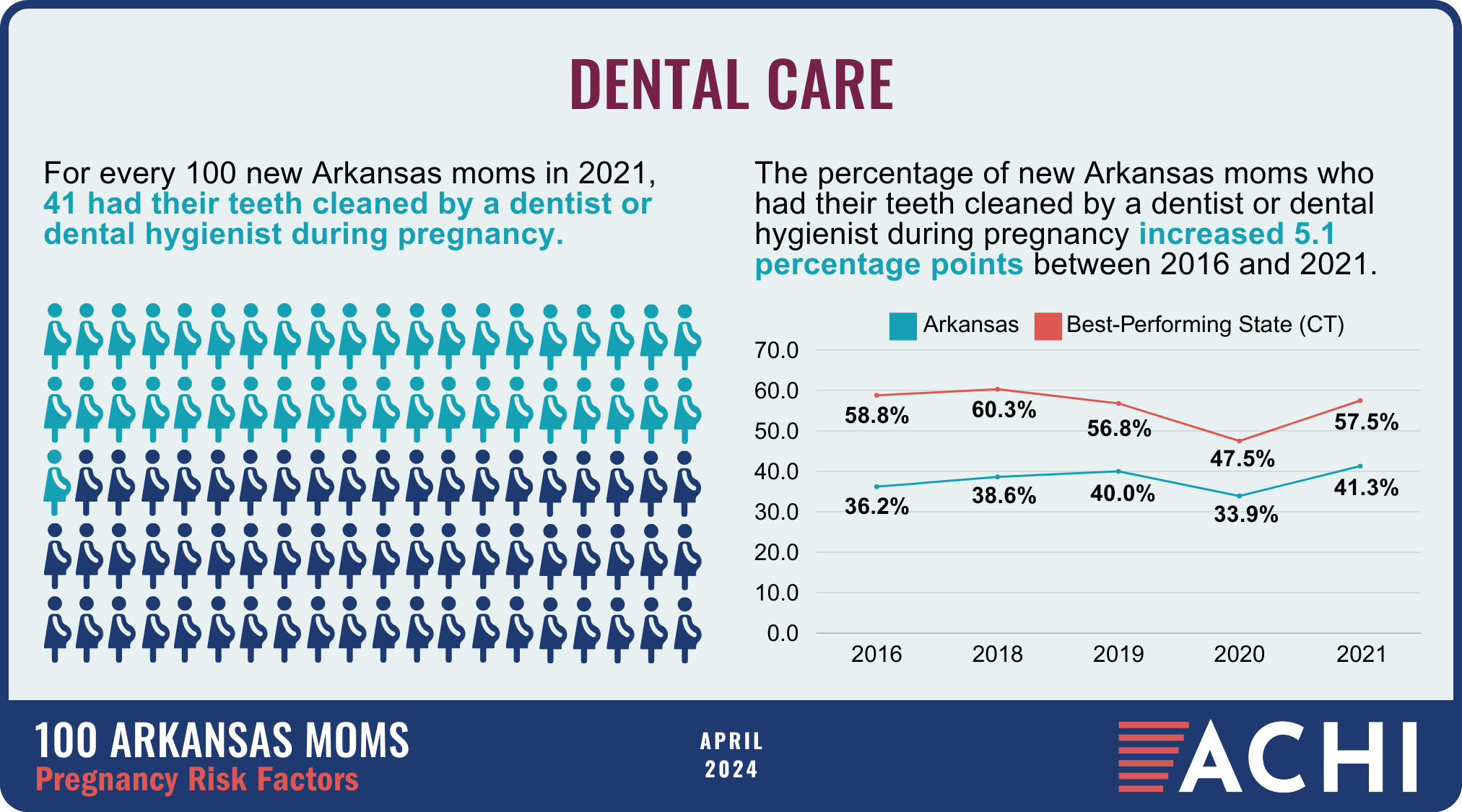
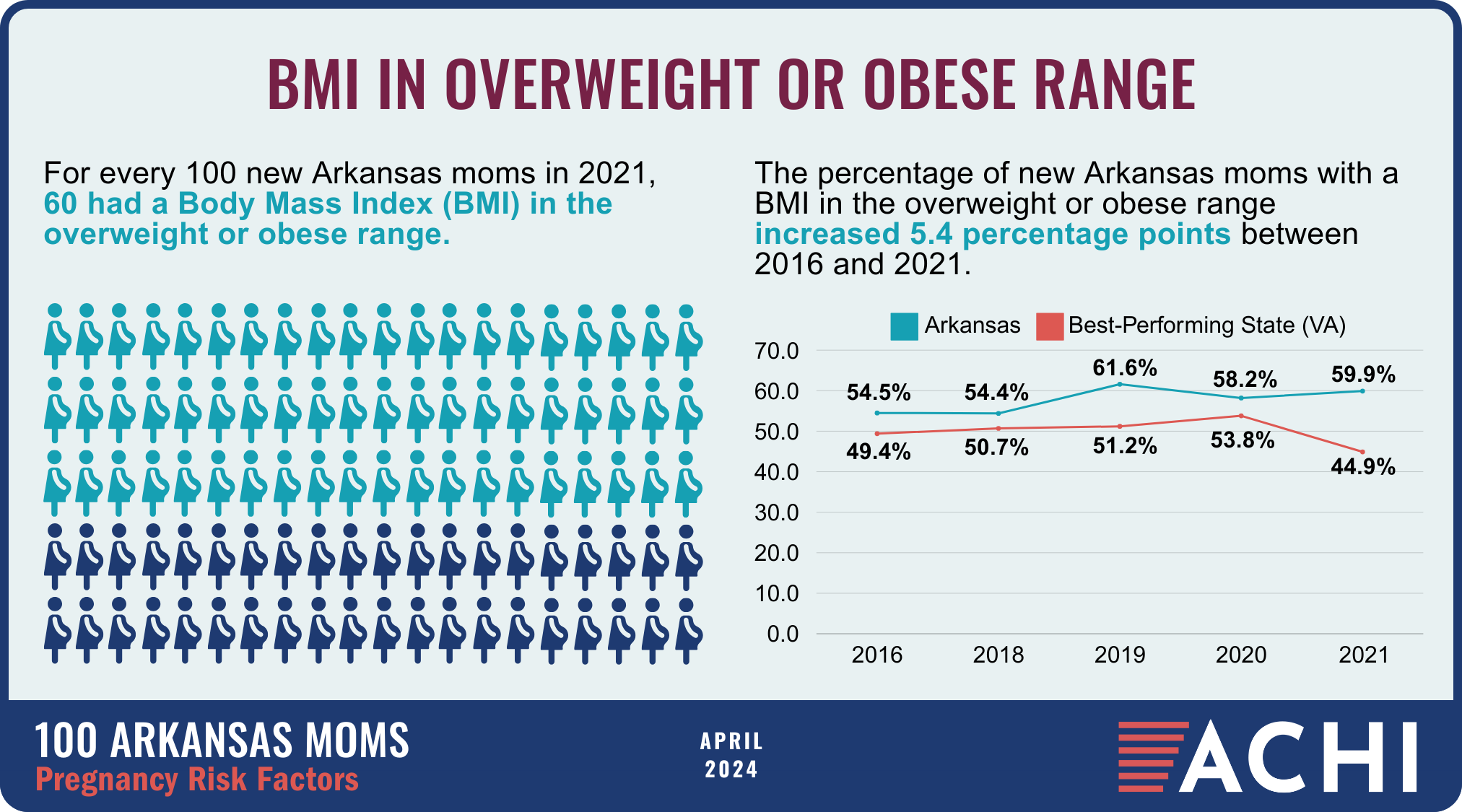

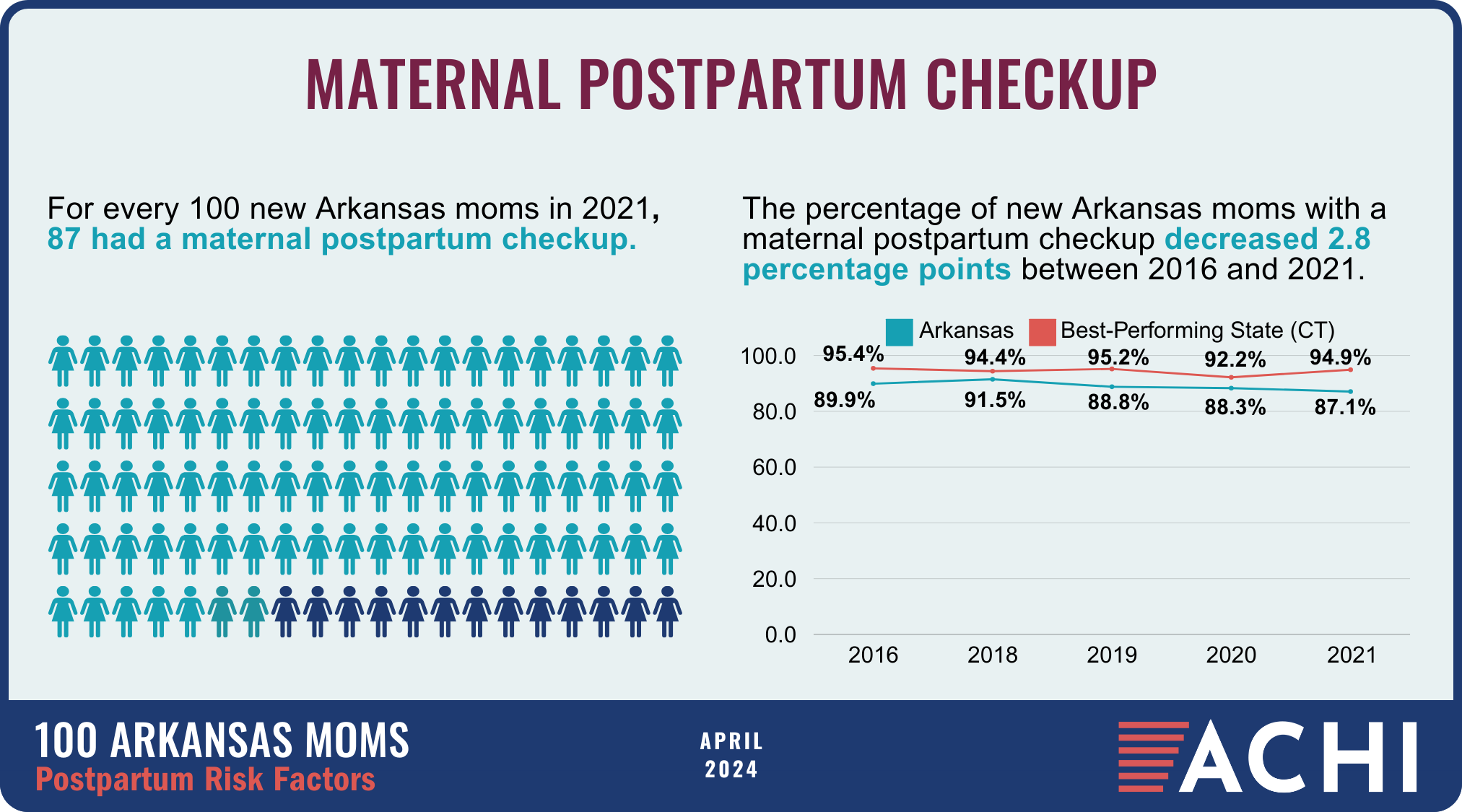
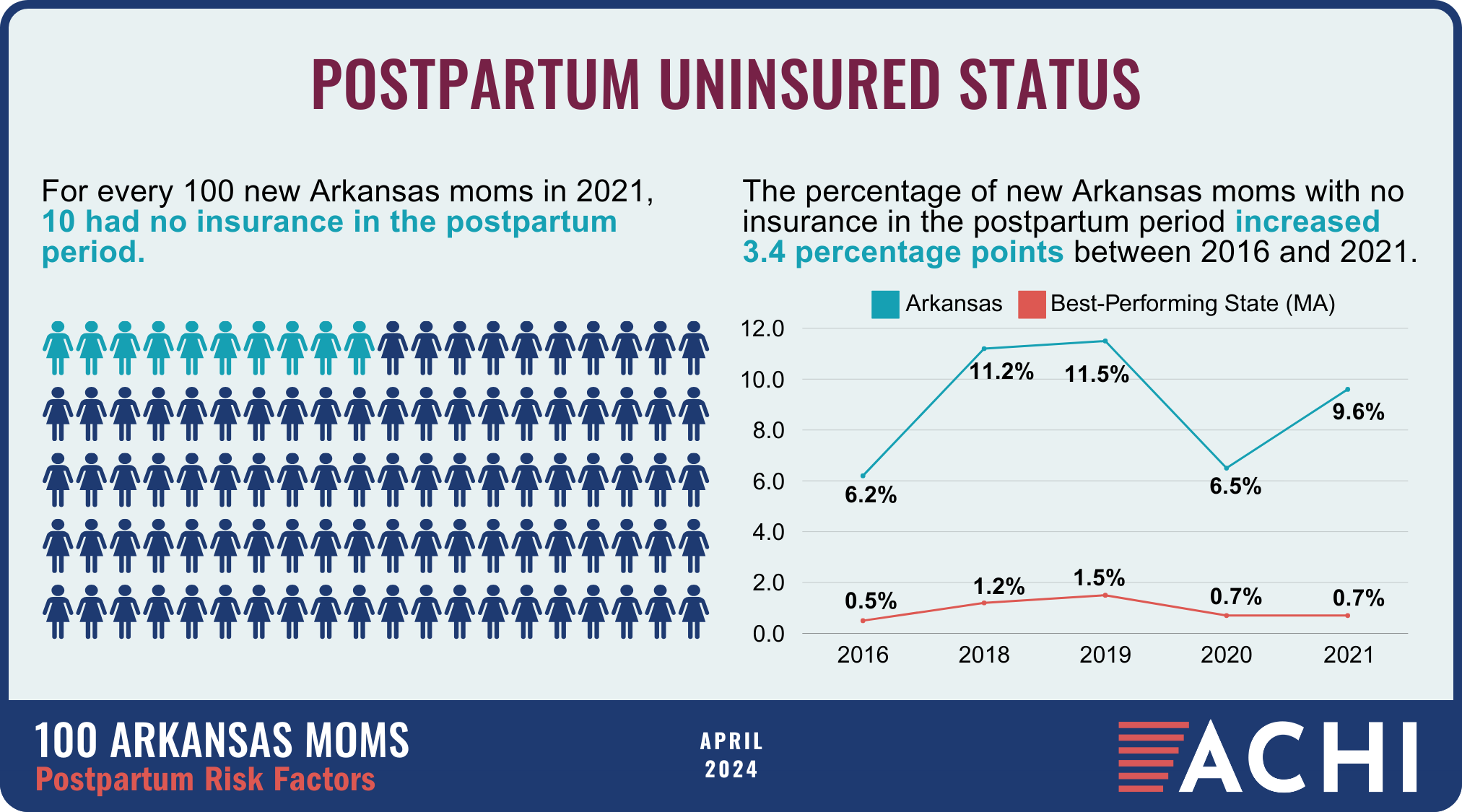
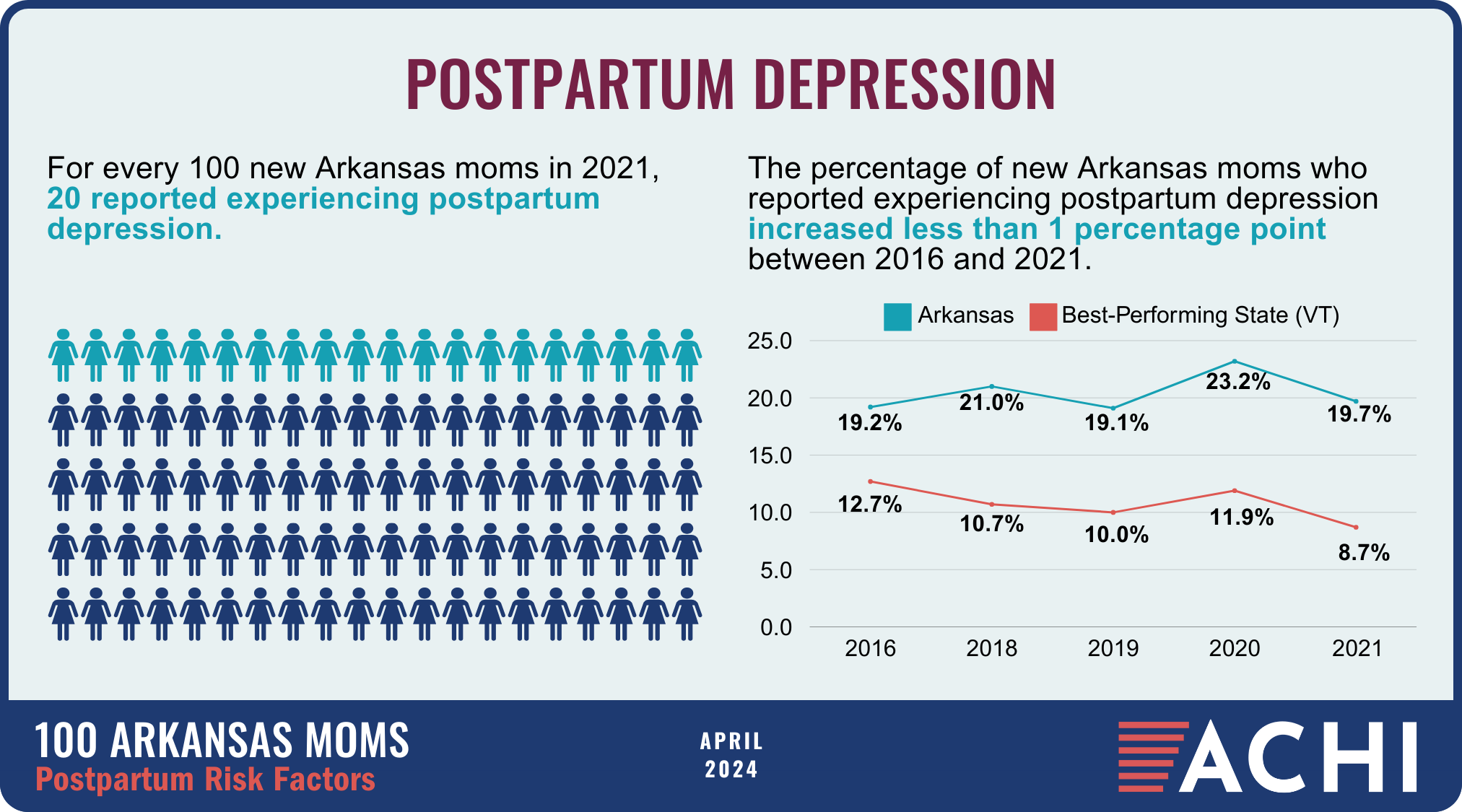
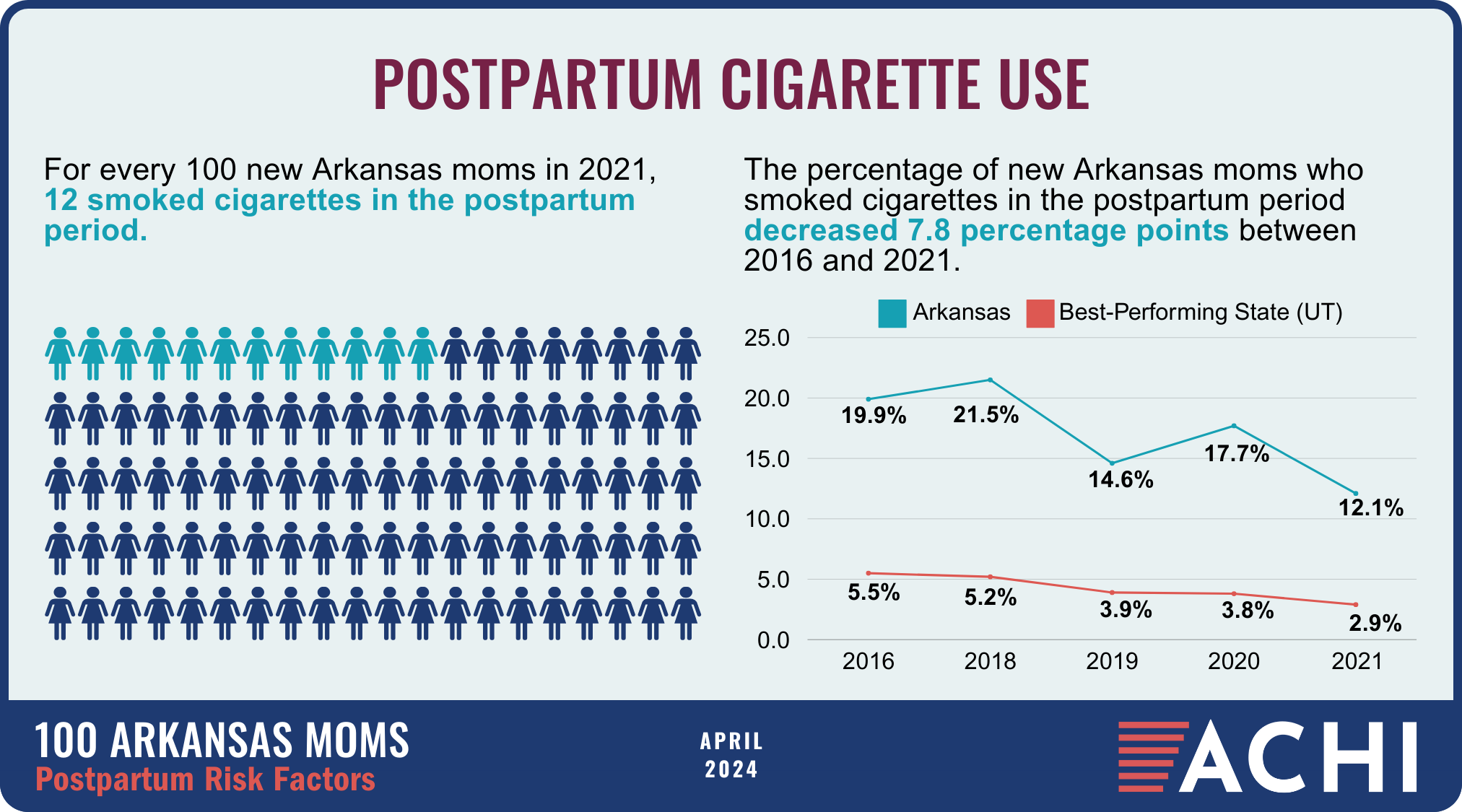
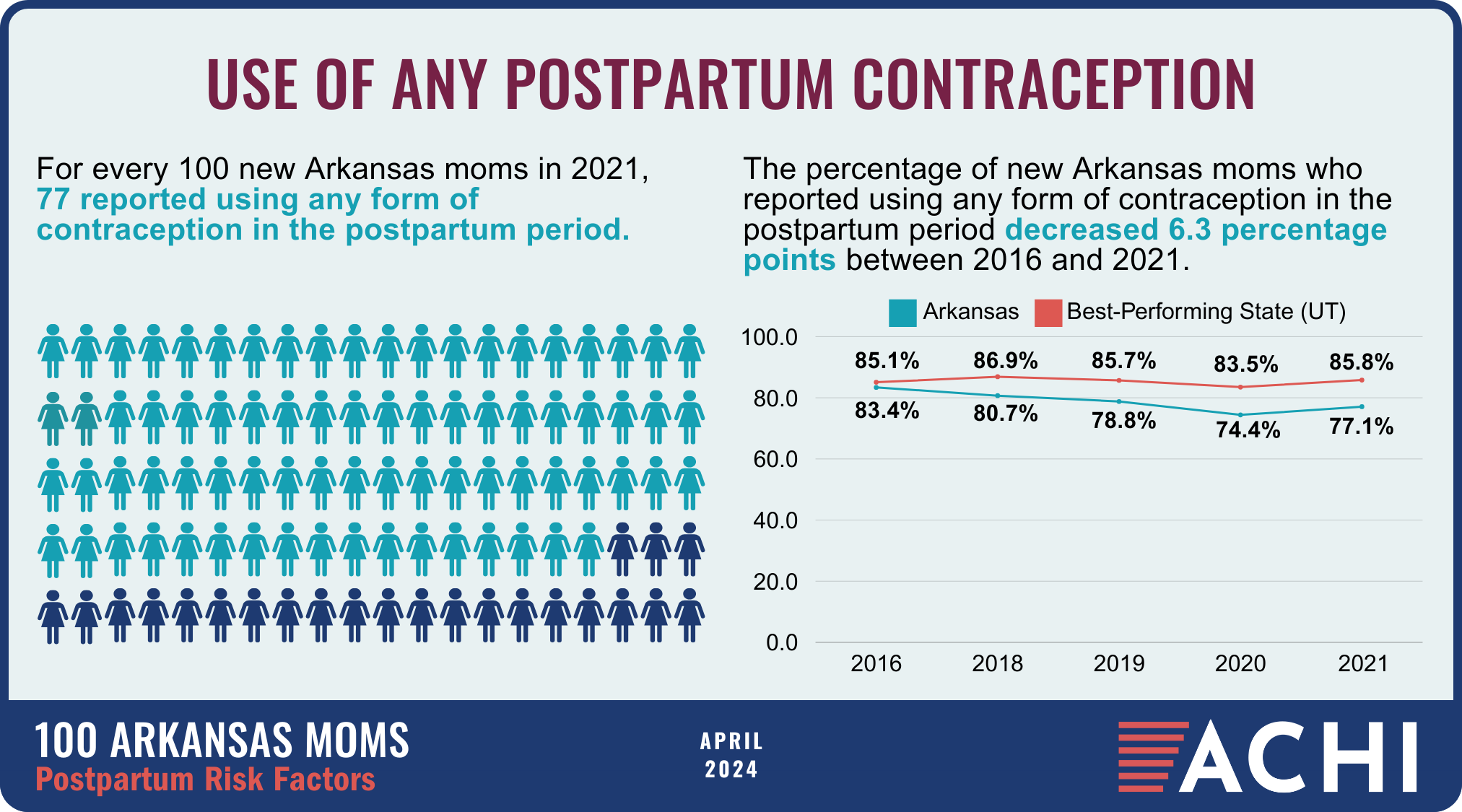
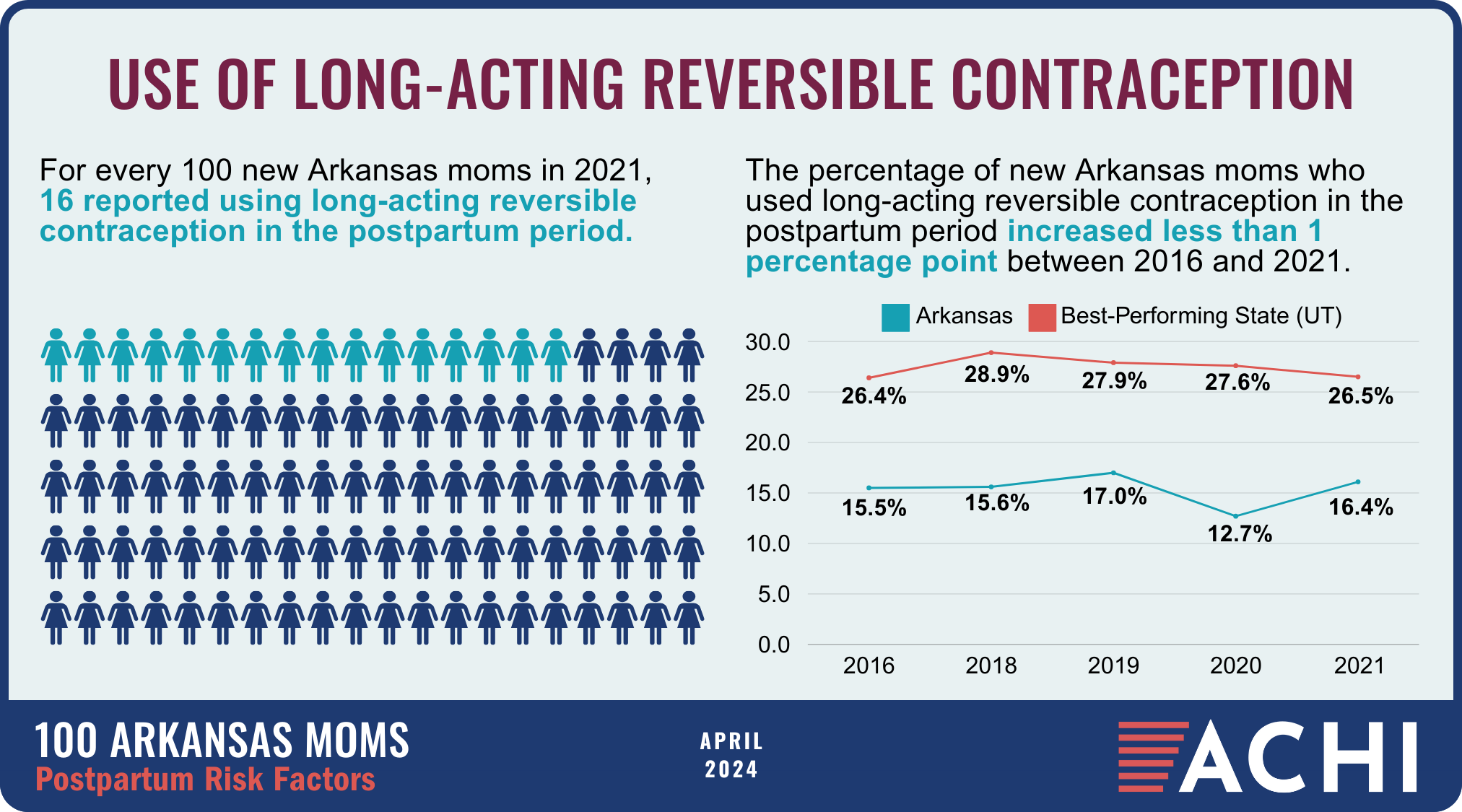
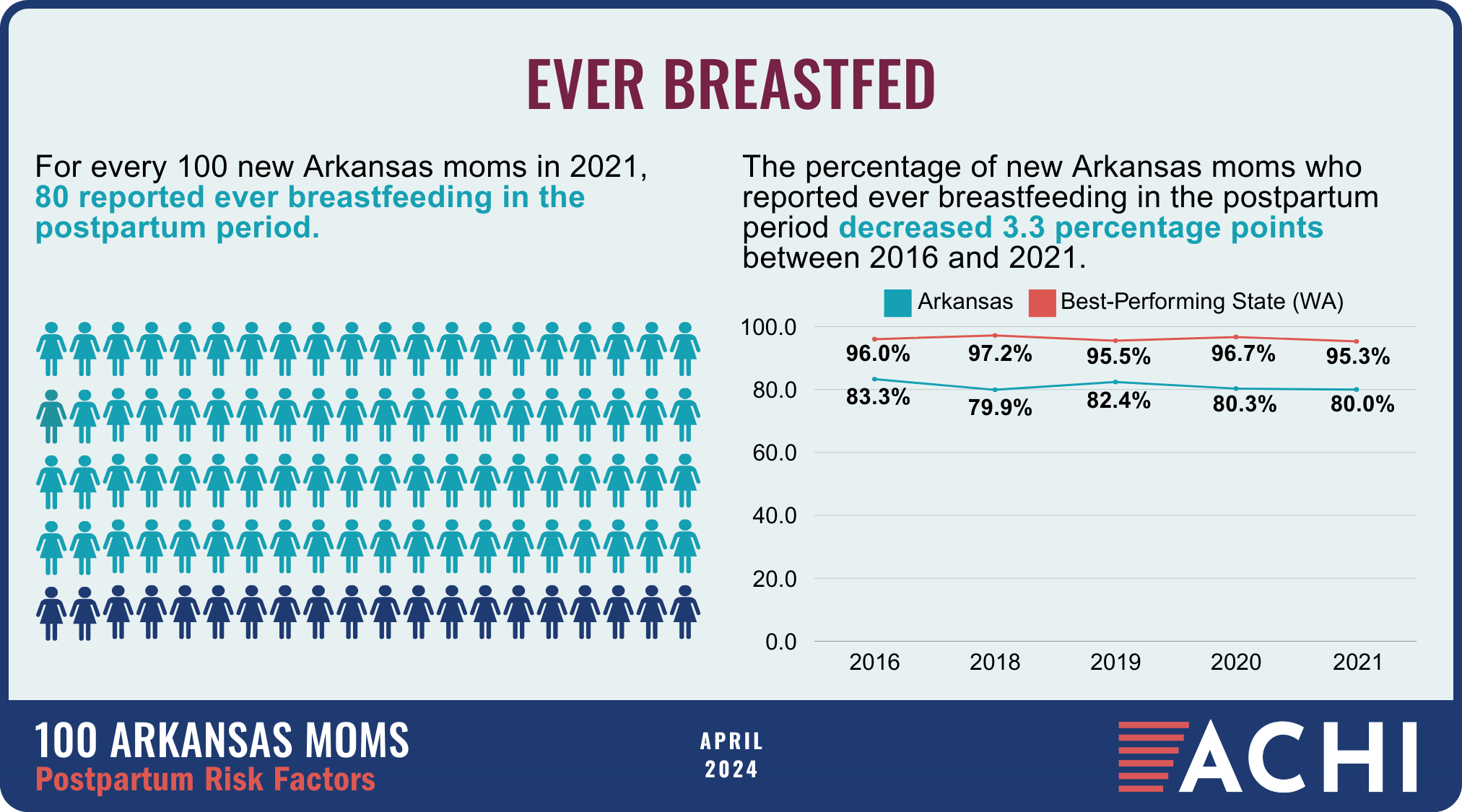
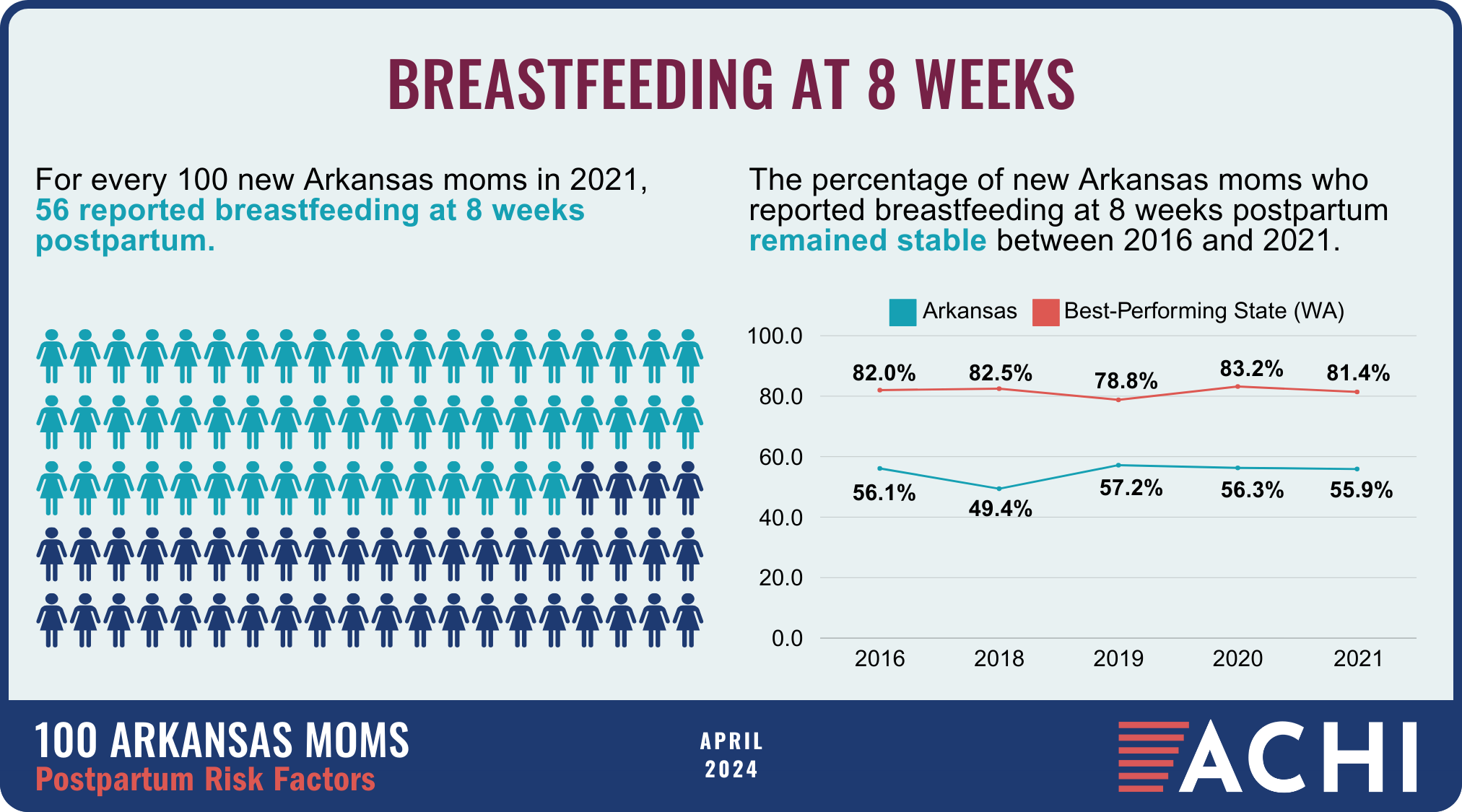
Data for the infographic are from the Centers for Disease Control and Prevention’s Pregnancy Risk Assessment Monitoring System. New moms are defined as women who gave birth two to four months prior to survey administration. Arkansas data for 2017 were not available.
Birthing Hospitals in Arkansas
More than half of rural hospitals in the U.S. no longer offer labor and delivery services, according to a report by the Center for Healthcare Quality and Payment Reform. At many hospitals that continue to offer labor and delivery services, those services are at risk due to challenges with the healthcare workforce and hospital finances that increasingly make it difficult to subsidize these departments, which are required to remain fully staffed 24 hours a day, seven days a week.
ACHI has identified 33 Arkansas hospitals that provide labor and delivery services. Seven hospitals in the state have closed their obstetric units since 2019. Among the state’s rural hospitals, 60% do not offer these services, which means expecting mothers must travel farther to deliver a child and receive appropriate prenatal and postpartum care, key points on a healthy birthing journey.
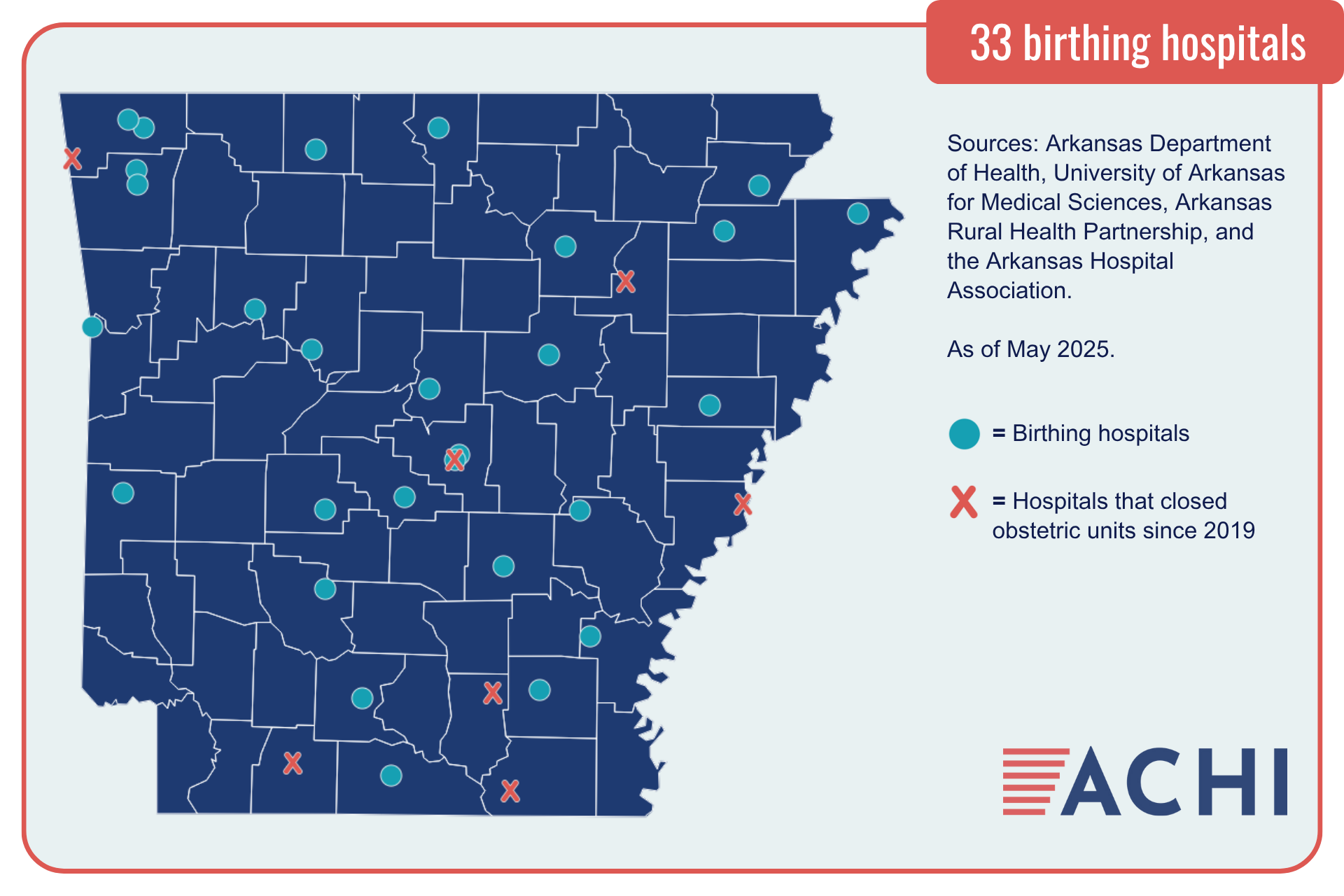
As of February 2025, Arkansas hospitals that provide labor and delivery services include:
- Arkadelphia: Baptist Health Medical Center
- Batesville: White River Medical Center
- Benton: Saline Memorial Hospital
- Bentonville: Northwest Medical Center
- Blytheville: Great River Medical Center
- Camden: Ouachita County Medical Center
- Clarksville: Johnson Regional Medical Center
- Conway: Baptist Health Medical Center
- Conway: Conway Regional Health System
- Dumas: Delta Memorial Hospital
- El Dorado: South Arkansas Regional Hospital
- Fayetteville: Washington Regional Medical Center
- Forrest City: Forrest City Medical Center
- Fort Smith: Baptist Health
- Fort Smith: Mercy Hospital Fort Smith
- Harrison: North Arkansas Regional Medical Center
- Hot Springs: CHI St. Vincent Hot Springs
- Hot Springs: National Park Medical Center
- Johnson: Willow Creek Women’s Hospital
- Jonesboro: NEA Baptist Memorial Hospital
- Jonesboro: St. Bernards Medical Center
- Little Rock: Baptist Health Medical Center
- Little Rock: University of Arkansas for Medical Sciences
- Mena: Mena Regional Health System
- Monticello: Baptist Health Medical Center – Drew County
- Mountain Home: Baxter Regional Medical Center
- North Little Rock: Baptist Health Medical Center
- Paragould: Arkansas Methodist Medical Center
- Pine Bluff: Jefferson Regional Medical Center
- Rogers: Mercy Hospital Northwest Arkansas
- Russellville: Saint Mary’s Regional Health System
- Searcy: Unity Health White County Medical Center
- Stuttgart: Baptist Health Medical Center
Travel Time to Delivery Facilities for Arkansas Mothers
Closures of labor and delivery services at Arkansas hospitals in recent years have led to longer travel times for many Arkansas mothers. Increased travel times to delivery facilities have been associated with higher risks of adverse maternal and neonatal outcomes. ACHI reviewed data on birth events occurring from 2016 to 2022 to estimate the travel times to delivery facilities for Arkansas mothers.
Our findings are presented in this infographic, which focuses on what we have identified as the fourth step of a healthy birthing journey: accessing safe delivery options.

- The statewide median minutes traveled to delivery facilities in 2022 was 16 minutes, but a look at mothers’ median travel times by county of residence found that travel times ranged from as short as 2 minutes to as long as 73 minutes.
- In some counties, increases in median travel times for residents followed the closure of local labor and delivery units. The infographic highlights Columbia and Phillips counties as examples of this phenomenon.
- The percentages of mothers facing extended travel times for delivery services have increased, with 28% of mothers traveling 30 minutes or more in 2022, up from 26% in 2016, and 8% of mothers traveling 60 minutes or more in 2022, up from 7% in 2016.
The data sources for these analyses were Arkansas Department of Health birth records (for in-state births) and the Arkansas Healthcare Transparency Initiative’s All-Payer Claims Database (for out-of-state births). Travel times were estimated using mothers’ home ZIP codes and the addresses of delivery facilities.
Interviews
Most postpartum mothers in Arkansas who experience an acute mental health or other behavioral health event requiring an emergency room visit or inpatient stay do not have a follow-up outpatient visit, an ACHI analysis finds. ACHI’s Dr. Joe Thompson discussed our findings related to Northwest Arkansas with Fayetteville-based public radio station KUAF.
Public radio station KUAF also looked the role doulas could play in addressing this crisis in a story featuring interviews with ACHI’s Dr. Joe Thompson, Willow Creek Women’s Hospital CEO Juli McWhorter, and Melissa Eudey, a certified doula. Doulas are professionals trained in childbirth who provide emotional, physical, and other supports to pregnant or recently pregnant woman. For more on what doulas do, see our explainer.
In 2023, radio station KUAF conducted three interviews with ACHI’s Dr. Joe Thompson for a series exploring in depth Arkansas’s high rate of maternal mortality. In the first episode, Dr. Thompson offers a general overview and discusses health issues prior to delivery. The second and third episodes focus on health issues during delivery and postpartum.
Related Blog Posts
How Doulas Could Help Address Arkansas’s Maternal Health Crisis
92% of Pregnancy-Related Deaths in Arkansas Likely Preventable
Report: Labor and Delivery Services in Jeopardy at Rural Arkansas Hospitals
CMS Launches Maternal Care Model Aimed at Improving Health Outcomes
Related Podcasts
Giving Birth in America: Arkansas
Arkansas had the highest maternal mortality rate across the United States as of early 2023. As the country faces a maternal health crisis, Every Mother Counts explored what that looks like on the ground by sharing the personal stories of three new Arkansas mothers in this recent documentary, Giving Birth in America: Arkansas.