Author
Jennifer Wessel, JD, MPH
Senior Policy Analyst and Data Privacy Officer
Contact
ACHI Communications
501-526-2244
jlyon@achi.net
Soaring costs have created a challenging financial environment for Arkansas hospitals, even prompting some to ask the Arkansas General Assembly for funding to keep their doors open. An interactive online tool created by the National Academy for State Health Policy (NASHP) provides a window into the costs that are stressing hospitals in Arkansas and across the nation.
NASHP’s Hospital Cost Tool, unveiled in April 2022 and recently updated, includes information on 73 Arkansas hospitals. Among other things, the tool shows that:
- In 2021, the median net patient revenue per adjusted patient discharge for Arkansas was $8,943. The national median was $13,454.
- In 2021, 27 Arkansas hospitals (37% of those reported) had a zero or negative margin. The median operating profit margin for Arkansas was 8%. The national median was 13%.
According to NASHP, its tool has been used to address healthcare consolidation, inform reimbursement rate negotiations, better understand hospital community benefit spending, and contribute to broader transparency efforts. The table below highlights several metrics displayed on the tool and the lowest-to-highest ranges for Arkansas hospitals. See the NASHP definitions below the table for more information about the metrics.
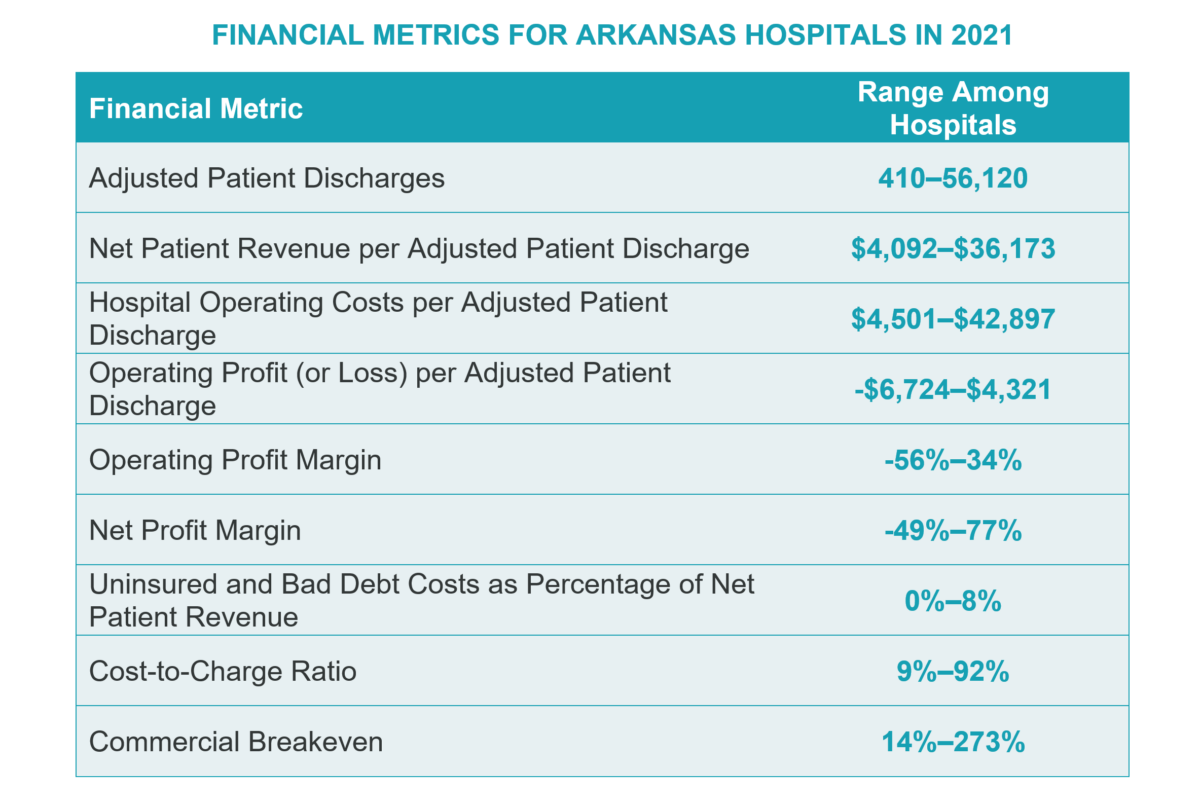
Adjusted Patient Discharges: The calculated inpatient and outpatient hospital discharges. The metric is computed by multiplying inpatient volume by an outpatient factor. The outpatient factor equals the total hospital charges divided by the inpatient hospital charges.
Net Patient Revenue: The gross patient charges, less contractual discounts, bad debt and charity care allowances, and other deductions agreed to by the hospital. Numbers are reported from the hospital’s accounting records.
Net Patient Revenue per Adjusted Patient Discharge: The net patient revenue divided by adjusted patient discharges, accounting for inpatient and outpatient volume.
Hospital Operating Costs: The portion of operating expenses related only to hospital patient care and eligible for reimbursement per Medicare federal regulations, sometimes referred to as Medicare allowed costs. Excluded operating expenses are referred to as Medicare disallowed costs.
Hospital Operating Costs per Adjusted Patient Discharge: The hospital operating costs divided by adjusted patient discharges, accounting for inpatient and outpatient volume.
Operating Profit (or Loss) per Adjusted Patient Discharge: The net patient revenue per adjusted patient discharge minus the hospital operating costs per adjusted patient discharge.
Operating Profit Margin: The operating profit (or loss) divided by net patient revenue. This metric represents the earnings on hospital patient services, excluding non-patient-related income and costs.
Net Income Profit Margin: The net income divided by net patient revenue, representing the percentage of net patient revenue retained by the hospital.
Uninsured and Bad Debt Costs as Percentage of Net Patient Revenue: The hospital operating costs for providing patient care to the uninsured or unpaid insured patients divided by net patient revenue, which presents the percentage of patient revenue received that the hospital applied to covering the costs of uninsured and bad debt patients.
Cost-to-Charge Ratio: The hospital operating costs reported as a percentage of the hospital’s charges. The charges are the list prices set by the hospital, similar to the manufacturer’s suggested retail price in other markets.
Commercial Breakeven: The payment level required from commercial payers (expressed as a percentage of Medicare rates) to allow the hospital to cover maximum hospital expenses, with no profit, for hospital inpatient and outpatient services. The covered hospital expenses include commercial patient hospital operating costs, shortfall or overage from public health programs, charity care and uninsured patient hospital costs, Medicare disallowed costs, and hospital other income and expense.
NASHP’s Hospital Cost Tool was developed with the help of Rice University’s Baker Institute for Public Policy and Mathematica, with funding from Arnold Ventures.
The Hospital Cost Tool uses Medicare cost reports, which hospitals submit annually to the federal government for purposes of determining their Medicare reimbursable cost, to calculate hospital financial measures. Physicians are not required to file Medicare cost reports, and finances for hospital-affiliated physician groups may not appear on hospital reports. However, these groups often incur operating losses that are subsidized by hospitals but may not be reflected on Medicare cost reports. This may result in an overstatement of operating margins when analyzing Medicare cost reports. This represents a key limitation, among others, of the tool. The tool should be interpreted with caution.