As ACHI’s health policy director, I had the opportunity to attend the National Rural Health Association’s (NHRA) Critical Access Hospital Conference in Kansas City, Mo., this week and hear from national rural health experts, including physicians and hospital administrators who are persevering at a time when rural hospitals are struggling to survive. Having been born at a rural hospital in Fordyce, I have a strong interest in ensuring acute and primary care access in rural areas and advancing policies that will allow rural hospitals to innovate and evolve in order to “right-size” for the health needs of the communities they serve.
Highlights of the conference included:
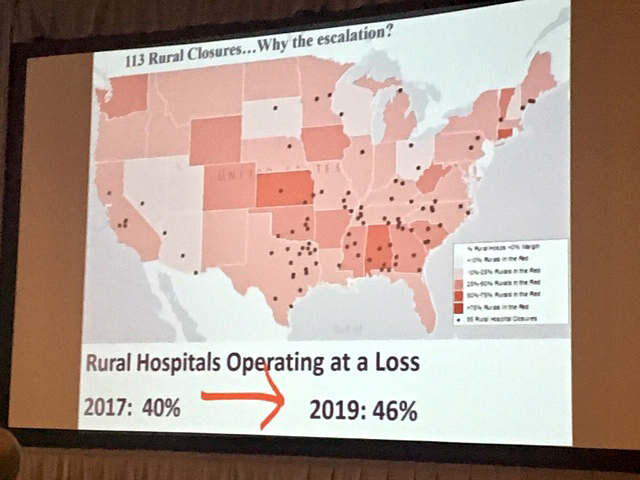
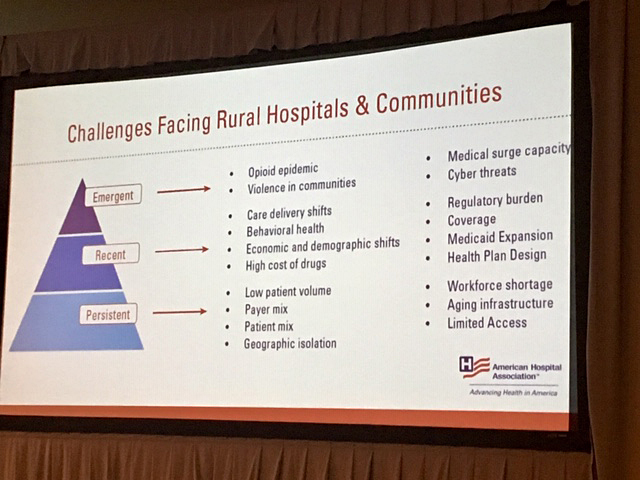
- NHRA Vice President for Government Affairs and Policy Director Maggie Elehwany noted renewed awareness of rural health issues and discussed key policy efforts to address rural hospital closures, provide flexibility and support to rural health clinics, and modernize health professional shortage designation criteria. She said rural health professionals and community leaders have welcomed federal grant funding to curb the opioid epidemic, but they have expressed concern that the funding restrictions do not permit them to address broader substance abuse issues, including methamphetamine abuse.
- Leslie Pelton, senior director of the Institute for Healthcare Improvement in Boston, spoke about age-friendly health systems that are guided by evidence-based practices for geriatric care, cause no harm to older adults, and are consistent with what matters most to older adults and their families. She said technology adaptation and the ability to demonstrate return on investment have proven to be barriers to rural hospitals, but technical assistance is available for hospitals seeking to be known as age-friendly.
- In a panel session on critical access hospitals responding to alternative payment models with downside risk, panelists noted the unique challenge for rural hospitals that have small margins and serve populations with greater health risks. Tim Putnam, president and CEO of Margaret Mary Community Hospital in Batesville, Ind., noted that rural hospitals can be nimble compared to larger health systems. “Righting quality metrics in a large system is like trying to steer a cruise ship. We’re more like a ski boat, and we can change direction in one staff meeting,” he said.
There was a great deal of discussion about a new rural hospital initiative expected to be announced in the fall by the Center for Medicare and Medicaid Innovation. The initiative is expected to include technical assistance and seed funding to support operational and financial transitions of rural hospitals.