
The United States has higher maternal and infant mortality rates than most other advanced economies. A new report from the Center for Healthcare Quality and Payment Reform assessing the state of maternal health care in the nation’s rural communities reveals persistent challenges, including in Arkansas. The report focuses on the health risks mothers in rural communities face due to limited access to care.
Fewer Rural Hospitals Offering Maternity Care
According to the report, over 80% of pregnancy-related deaths are preventable with proper prenatal, labor and delivery, and postpartum care. A major challenge lies in rural areas where many hospitals no longer offer maternity services.
Since 2020, 14% of the labor and delivery units at rural Arkansas hospitals have closed, and about 28% are currently at risk of closing, according to the report.
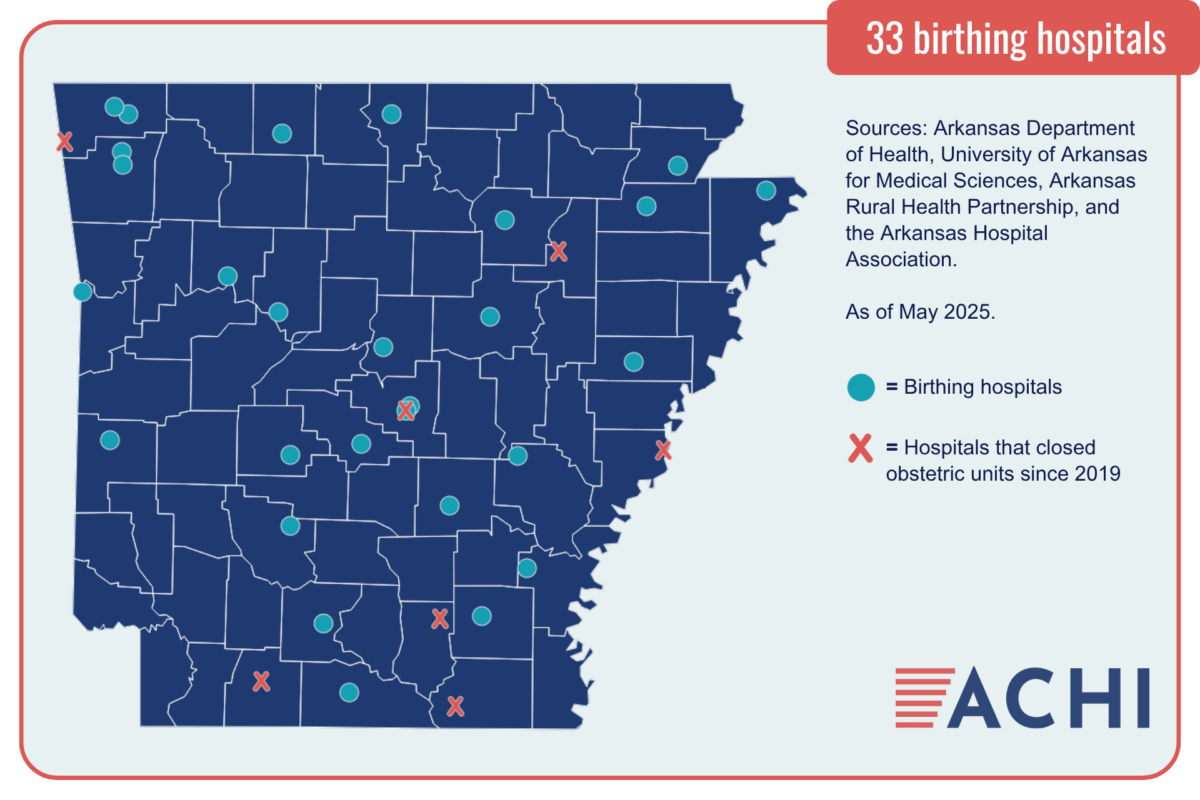
ACHI’s map of birthing hospitals (above) shows that only 33 hospitals in Arkansas continue to provide labor and delivery services as of May 2025. Since 2019, seven hospitals have closed their obstetric units, four of them due to staffing shortages and three due to financial considerations.
Financial Pressures on Rural Hospitals
The threat to rural maternity care is part of a broader financial crisis facing rural hospitals. Many of these hospitals are losing money on other services such as emergency care and primary care, which threatens their ability to stay open regardless of how well maternity care is funded.
In Arkansas, 50.6% of births are paid for by private insurance and 41% are paid by Medicaid. Health plans often pay rural hospitals less than the actual cost of providing maternity care, potentially undermining the financial sustainability of maternity units and contributing to workforce recruitment challenges in obstetrics.
Maintaining high-quality, safe maternity care requires having providers who can assist women with vaginal deliveries and cesarean sections on a 24/7 basis. As the Center for Healthcare Quality and Payment Reform’s report notes, obstetricians and family physicians are increasingly unable or unwilling to be on call at all hours. In response, hospitals must employ more physicians, change their methods of staffing, or contract with additional physicians to cover on-call shifts.
Rural hospitals in Arkansas also face pressure from rising staff expenses, fewer births due to the out-migration of younger people from rural areas of the state, and Medicaid reimbursement rates for obstetric care that are 30% lower than Medicare.
These financial pressures are especially difficult in communities with higher numbers of low-income residents. Addressing these pressures is essential to making childbirth safer for mothers across Arkansas.
Statewide Efforts and Initiatives
Act 124 of 2025, the Healthy Moms, Healthy Babies Act, is a step toward increasing access to prenatal, labor and delivery, and postpartum care for Arkansas mothers. The act establishes presumptive Medicaid eligibility for pregnant women, allowing them to receive Medicaid benefits and initiate prenatal care while waiting for their Medicaid applications to be approved; establishes Medicaid coverage for pregnancy-related health monitoring; and unbundles Medicaid payments for pregnancy care, allowing providers to be paid for up to 14 prenatal and postnatal care visits.
In addition, the federal Transforming Maternal Health Model Grant Program will provide Arkansas with $17 million over the next 10 years to support maternal health care improvements. The Transforming Maternal Health Model, a whole-person approach to pregnancy, childbirth, and postpartum care, is aimed at reducing disparities in access and treatment, improving outcomes and experiences for mothers and their newborns, and reducing overall expenditures.






