Author
Elizabeth (Izzy) Montgomery, MPA
Policy Analyst
Contact
ACHI Communications
501-526-2244
jlyon@achi.net
A new analysis from the U.S. Department of Health and Human Services’ Office of the Inspector General finds that Medicare and Medicaid enrollees in many high-needs areas of the country — including several counties in Arkansas — lack access to medications for opioid use disorder (MOUD).
Background
The U.S. Food and Drug Administration has approved three drugs used in MOUD: buprenorphine, methadone, and naltrexone. Buprenorphine is a controlled substance accessible through office-based buprenorphine providers (e.g., primary care providers) and opioid treatment programs. Methadone is also a controlled substance that reduces opioid cravings and withdrawal by blunting or blocking the effects of opioids. Methadone can only be administered or dispensed by opioid treatment programs certified by the Substance Abuse Mental Health Services Administration (SAMSHA) in an outpatient setting, and patients are usually required to visit programs daily to receive their methadone dose. However, federal regulations were amended in 2024 to allow certain patients to have up to 28 take-home doses provided to them. Naltrexone is not a controlled substance and can be prescribed by any qualified healthcare provider, but requires seven to 14 days of opioid abstinence before it can be initiated and has lower rates of medication adherence.
A law passed by Congress in 2020 added opioid treatment program coverage requirements to Medicare and requires that state Medicaid programs cover all forms of MOUD treatment. The law also expanded coverage for Medicare enrollees to include MOUD services provided by an opioid treatment center and waived cost sharing for these services.
The Office of the Inspector General notes that previous work found that many Medicare and Medicaid enrollees with opioid use disorder did not receive MOUD through these programs. While access to these programs has been expanded, this analysis focused on providers and the extent to which they prescribed or administered MOUD services and whether they were located in high-need areas. The report also includes a companion product with interactive maps using county- and state-level data. The maps below highlight findings specific to MOUD providers and treatment availability in Arkansas.
Key Findings
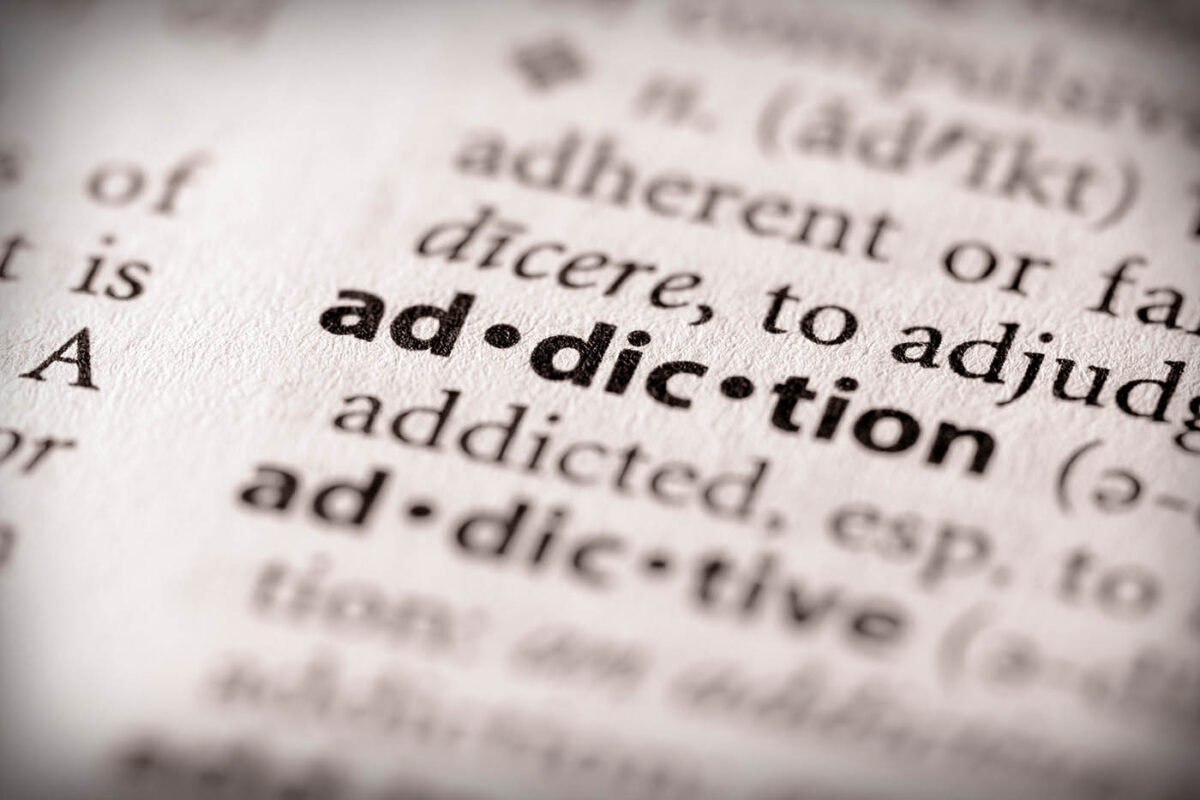
- In 2022, 19% of U.S. counties did not have a single MOUD provider, including more than 100 counties with high needs for MOUD services. This includes 14 Arkansas counties, as shown in Figure 1 below. Additionally, more than one-quarter of high-need counties in the U.S. had few or no MOUD providers, including 27 counties in Arkansas (see Figure 1).
- Nationally, 1,258 counties were in high need of MOUD services due to their disproportionately high rates of drug overdose deaths, with 586 of those counties also deemed to be socially vulnerable and at greater risk of public health emergencies due to socioeconomic and household demographic factors. Eleven counties in Arkansas were determined to have both a high need (based on drug overdose deaths) and high social vulnerability (based on the Centers for Disease Control and Prevention/Agency for Toxic Substances and Disease Registry Social Vulnerability Index, which uses 16 U.S. Census Bureau variables to identify communities particularly vulnerable to the negative impacts of external stresses on human health, such as the opioid crisis). Those counties are Fulton, Mississippi, Poinsett, Cross, Monroe, Pulaski, Garland, Scott, Miller, Union, and Bradley counties. Poinsett County is a particular outlier in Arkansas because it is the only county in the state with few MOUD providers (only three), a high need for MOUD services, and high social vulnerability.
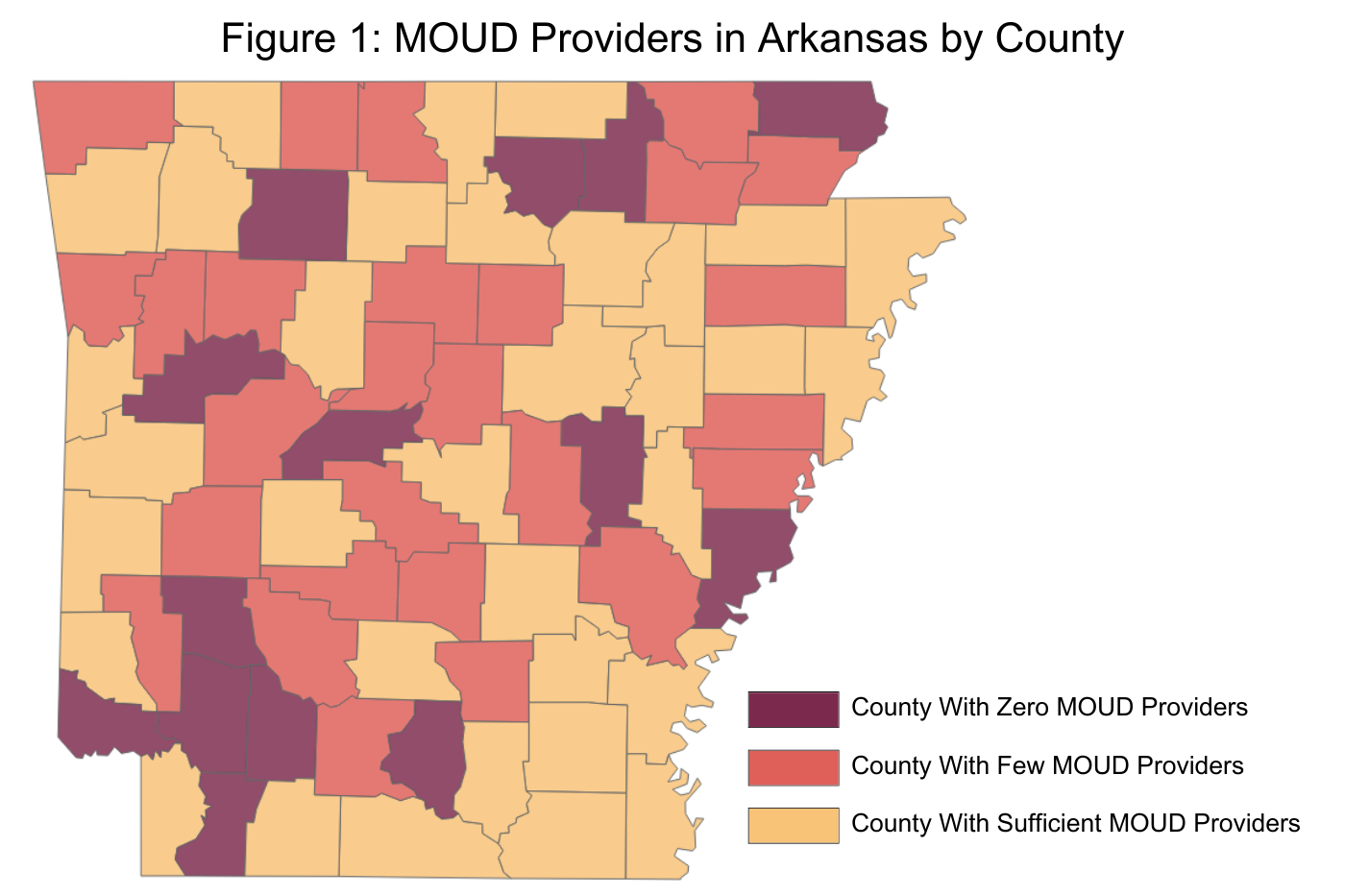
- Nearly one-third (32%) of U.S. counties did not have a single MOUD provider that treated any Medicare or Medicaid enrollees. There was considerable overlap, with the study finding that of counties with no MOUD providers treating Medicaid enrollees, 95% of those counties also had no MOUD providers treating Medicare enrollees. Figure 2 shows the distribution of Medicaid MOUD providers by county in Arkansas. Although not shown here, the distribution of MOUD providers for Medicare enrollees was very similar.
- In Arkansas, 40% of opioid treatment centers prescribed or administered buprenorphine or methadone to at least one Medicare enrollee in 2022 (below the national average of 77%), compared to 34% of office-based buprenorphine providers who prescribed or administered buprenorphine to at least one Medicare enrollee (above the national average of 28%).
- Among Arkansas Medicaid enrollees, 20% of opioid treatment providers prescribed or administered buprenorphine or methadone to at least one Medicaid enrollee in 2022 (below the national average of 77%), compared to 35% of office-based buprenorphine providers who prescribed or administered buprenorphine to at least one Medicaid enrollee (below the national average of 38%).
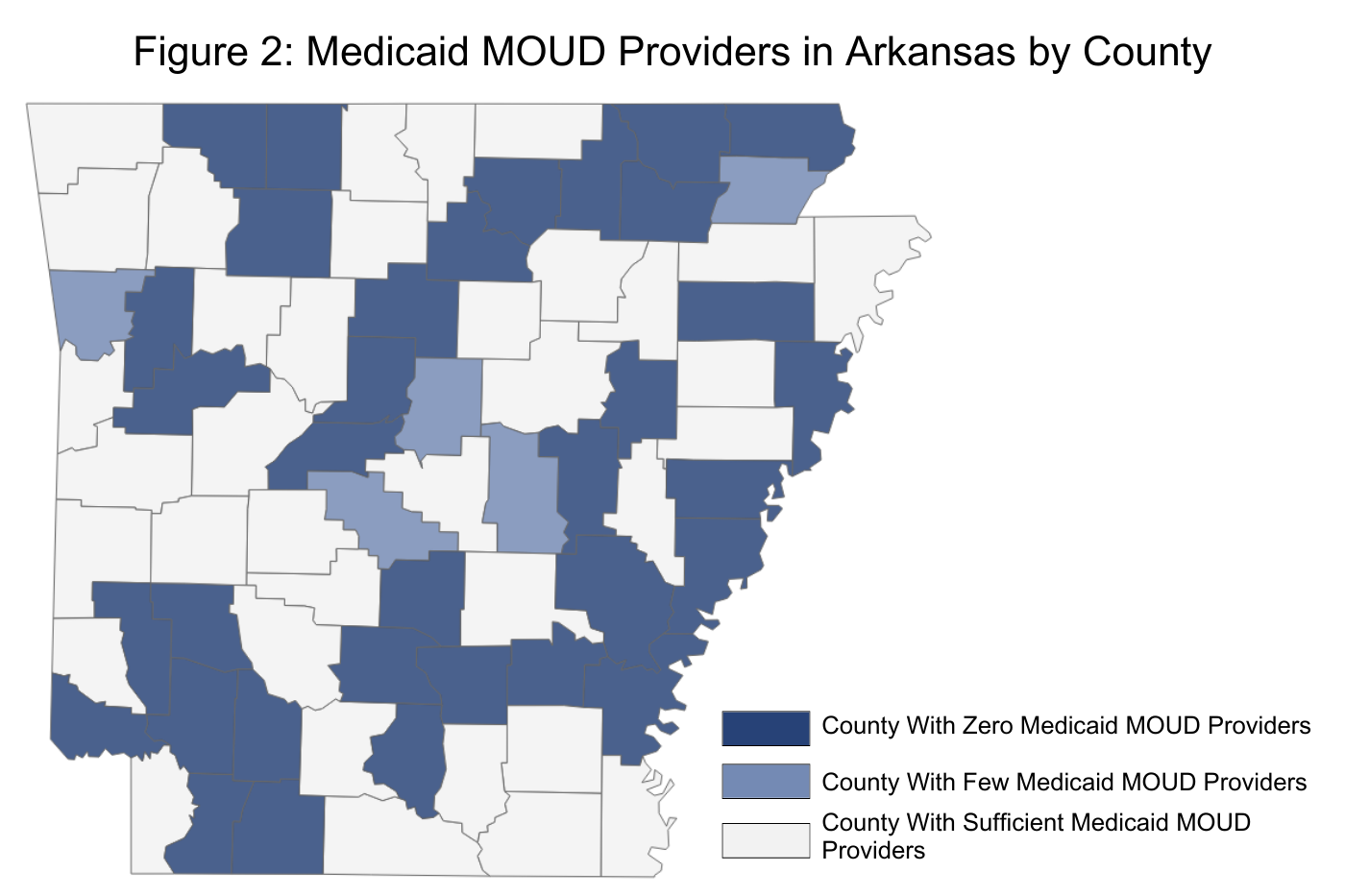
- Only four counties in Arkansas had opioid treatment programs and all four were in urban areas (Pulaski, Saline, Crawford, and Miller), which reveals disparities in access to these programs in rural counties. Fourteen counties in Arkansas had no office-based buprenorphine providers (see Figure 3).
Report Recommendations
Recommendations for the Centers for Medicaid and Medicare Services cited in the report include:
- Targeting efforts geographically to increase the number of MOUD providers who deliver treatment to both Medicare and Medicaid enrollees in high-need counties.
- Working with states to assess whether their Medicaid reimbursement rates for MOUD treatments are sufficient to recruit and retain sufficient MOUD providers.
- Working with SAMHSA to develop and maintain a list of active office-based buprenorphine providers.
Provisional data from the Centers for Disease Control and Prevention found that in 2023, national drug overdose deaths declined for the first time in five years. Arkansas experienced a nearly 13% decrease in drug overdose deaths in 2023 compared to 2022 (517 deaths vs. 591 deaths, respectively).
ACHI analyses has also shown decreasing trends in opioid prescription fills, with the number of Arkansans filling such prescriptions declining 35% from 2017 to 2022. Our analyses also show a significant increase in naloxone prescriptions resulting from Act 651 of 2021, which requires a co-prescription of naloxone in certain situations (when an opioid prescription of 50 or more morphine milligram equivalents per day is prescribed). Between fiscal years 2021 and 2022, there was a 366% surge in naloxone prescription fills and a 340% increase in enrollees who filled a naloxone prescription.