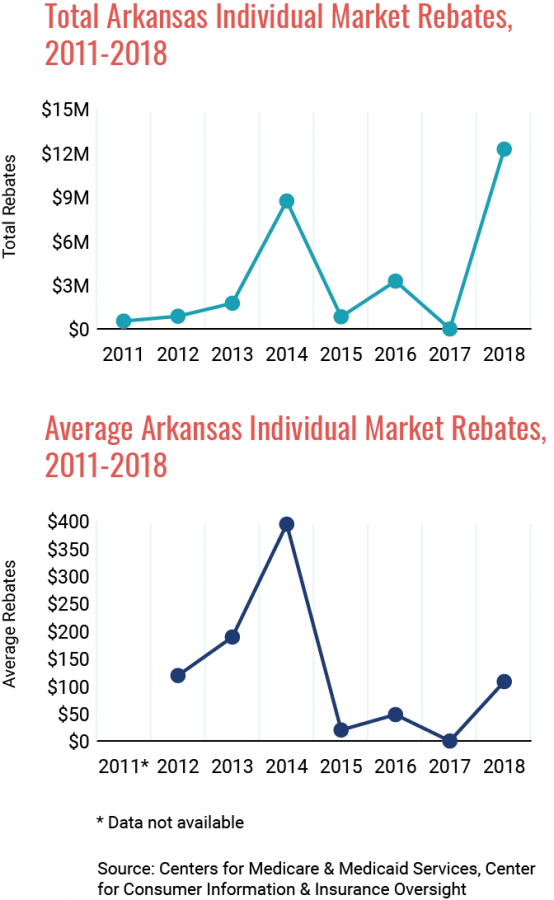
 Health insurer Centene issued $12,251,429 in medical loss ratio (MLR) rebates to individual market insurance purchasers in Arkansas for the 2018 reporting year, according to a report by the Centers for Medicare & Medicaid Services. Centene sells plans in Arkansas under the brand name Ambetter.
Health insurer Centene issued $12,251,429 in medical loss ratio (MLR) rebates to individual market insurance purchasers in Arkansas for the 2018 reporting year, according to a report by the Centers for Medicare & Medicaid Services. Centene sells plans in Arkansas under the brand name Ambetter.
Average rebates issued were $108. Roughly 80% of the premiums in the Arkansas individual market are paid for by the Medicaid program. Consequently, the majority of the rebates were issued to the Medicaid program.
The MLR requirement, or 80/20 rule, mandates that health insurers spend 80% of individual market premium revenues on medical claims and quality of care improvement efforts each reporting year. The remaining 20% can be used for administration, marketing, overhead, and profit. Health insurers that do not meet the 80% threshold must issue each purchaser a rebate in the form of a premium credit, a check, or the original payment method.
No other insurer offering individual marketplace plans in Arkansas fell short of the 80% threshold in 2018.
Note: The MLR requirement also applies to the small group and large group markets. However, the MLR threshold for large group plans is higher at 85%.