The rising cost of prescription drugs and the lack of transparency around drug pricing are issues impacting millions of Americans and receiving attention from policymakers at the federal and state levels. While the U.S. Department of Health and Human Services promotes a federal agenda to increase transparency and bring down prices, states are using local policy and data assets to pursue similar goals, as highlighted in two recent articles in the Journal of the American Medical Association on state drug transparency laws and cost containment efforts.
At the 34th annual meeting of the National Association of Health Data Organizations (NAHDO) in Little Rock in November, hosted by ACHI, a multi-state panel showcased initiatives by NAHDO partners in California, Maine, and Arkansas, offering a range of perspectives on efforts to improve pharmacy and drug cost transparency.
Maine
Maine’s prescription drug reporting under Public Law Chapter 406 requires the Maine Health Data Organization (MHDO) to produce annual prescription drug reports. These reports include the 25 costliest drugs, the most frequently used drugs, and the drugs with the highest year-to-year cost increases.
Enacted in 2019, Maine Public Law Chapter 470 seeks to further advance consumer awareness and pharmacy transparency by requiring that new pricing information be submitted by manufacturers, pharmacy benefit managers, and wholesale distributors.
California
California’s Office of Statewide Health Planning and Development (OSHPD) is responsible for collection and publication of prescription drug information, as well as administration of penalties when compliance issues arise.
Through the new Cost Transparency Rx (CTRx) Program, OSHPD collects information under California Senate Bill 17, which requires drug manufacturers to provide advance notice of drug cost increases to purchasers, along with information about the impacts of cost increases to health plans and insurers.
Arkansas
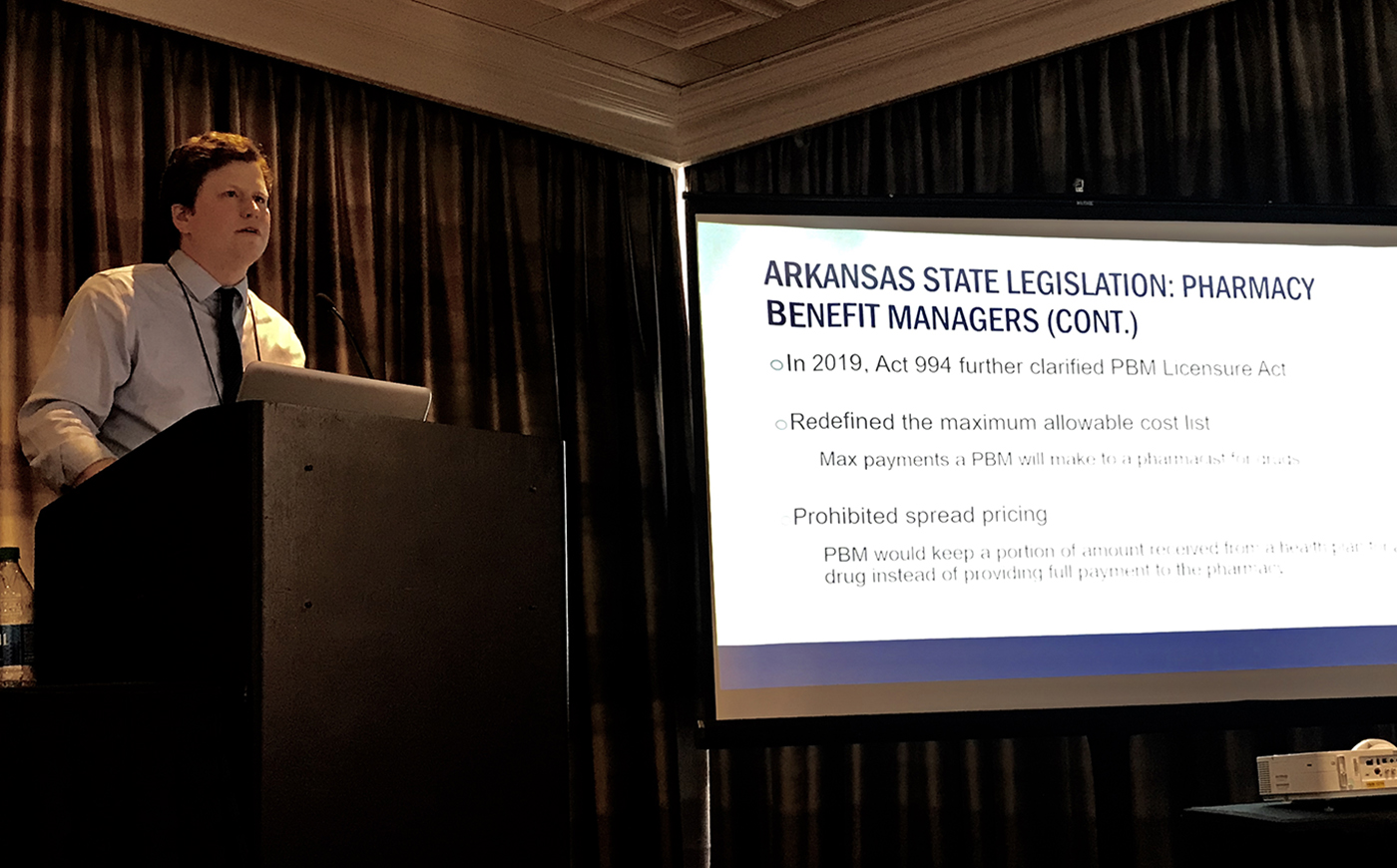
The Arkansas Pharmacy Benefit Licensure Act was passed in 2018, allowing the Arkansas Insurance Department to require that pharmacy benefit managers (PBMs) be licensed by the state and authorizing the department to review and approve PBM compensation programs with pharmacies.
Act 994 of 2019 clarified the licensure act by redefining maximum allowable costs and prohibiting spread pricing, the practice of a PBM keeping a portion of the amount it receives from a health plan for a drug instead of providing full payment to the pharmacy.
Researchers at ACHI have begun working directly with pharmacies to collect data to compare amounts paid for specific drugs to pharmacy claims submitted to the Arkansas All-Payer Claims Database. Preliminary analyses have revealed variation in amounts paid, with approximately 60% of payer-submitted amounts matching the amounts paid to pharmacies.
The rising cost of prescription drugs and the lack of transparency around drug pricing are issues impacting millions of Americans and receiving attention from policymakers at the federal and state levels. While the U.S. Department of Health and Human Services promotes a federal agenda to increase transparency and bring down prices, states are using local policy and data assets to pursue similar goals, as highlighted in two recent articles in the Journal of the American Medical Association on state drug transparency laws and cost containment efforts.
At the 34th annual meeting of the National Association of Health Data Organizations (NAHDO) in Little Rock in November, hosted by ACHI, a multi-state panel showcased initiatives by NAHDO partners in California, Maine, and Arkansas, offering a range of perspectives on efforts to improve pharmacy and drug cost transparency.
Maine
Maine’s prescription drug reporting under Public Law Chapter 406 requires the Maine Health Data Organization (MHDO) to produce annual prescription drug reports. These reports include the 25 costliest drugs, the most frequently used drugs, and the drugs with the highest year-to-year cost increases.
Enacted in 2019, Maine Public Law Chapter 470 seeks to further advance consumer awareness and pharmacy transparency by requiring that new pricing information be submitted by manufacturers, pharmacy benefit managers, and wholesale distributors.
California
California’s Office of Statewide Health Planning and Development (OSHPD) is responsible for collection and publication of prescription drug information, as well as administration of penalties when compliance issues arise.
Through the new Cost Transparency Rx (CTRx) Program, OSHPD collects information under California Senate Bill 17, which requires drug manufacturers to provide advance notice of drug cost increases to purchasers, along with information about the impacts of cost increases to health plans and insurers.
Arkansas
The Arkansas Pharmacy Benefit Licensure Act was passed in 2018, allowing the Arkansas Insurance Department to require that pharmacy benefit managers (PBMs) be licensed by the state and authorizing the department to review and approve PBM compensation programs with pharmacies.
Act 994 of 2019 clarified the licensure act by redefining maximum allowable costs and prohibiting spread pricing, the practice of a PBM keeping a portion of the amount it receives from a health plan for a drug instead of providing full payment to the pharmacy.
Researchers at ACHI have begun working directly with pharmacies to collect data to compare amounts paid for specific drugs to pharmacy claims submitted to the Arkansas All-Payer Claims Database. Preliminary analyses have revealed variation in amounts paid, with approximately 60% of payer-submitted amounts matching the amounts paid to pharmacies.