Contact
Joseph W. Thompson, MD, MPH
President & CEO
501-526-2244
achi@achi.net
Contact
Craig Wilson, JD, MPA
Director, Health Policy
501-526-2244
cwilson@achi.net
As we discussed in a previous blog post, Arkansas this year became the third state, after Kentucky and Indiana, to receive approval from the U.S. Department of Health and Human Services (HHS) to implement a work requirement for Medicaid adults. On June 1, Arkansas became the first state to implement such a requirement. After its first three months, the requirement has resulted in the termination of health care coverage for more than 4,000 people.
Arkansas Department of Human Services officials announced on Sept. 12 that 4,353 people who were enrolled in the state’s Medicaid expansion program had been locked out of coverage for failing to comply with the work requirement for three months. The agency has said those people will have until October 5 to apply for a good cause exemption if they were unable to access an online reporting portal because of network server issues that affected it and other agencies.
Kentucky intended to implement its work requirement July 1, but a federal judge in Washington, D.C., issued an order on June 29 temporarily blocking the requirement from taking effect. The judge found that the HHS Secretary had not adequately considered whether Kentucky’s work requirement would cause some Medicaid beneficiaries to lose coverage and whether it would promote the central goal of Medicaid, to “furnish medical assistance to citizens.”
Two of the groups that challenged Kentucky’s work requirement filed a lawsuit on August 14 in the same federal court seeking to halt Arkansas’ requirement. Like the lawsuit challenging Kentucky’s work requirement, the suit against Arkansas’ work requirement alleges that the HHS secretary granted approval without due consideration. Both suits also raise an argument that the judge did not initially reach in the Kentucky challenge: that the Centers for Medicare and Medicaid Services (CMS), in issuing a January 11, 2018, guidance announcing it would allow states to make “community engagement” a requirement for Medicaid beneficiaries, acted illegally because only Congress can establish new eligibility criteria for Medicaid.
CMS guidance states in part, “Subject to the full federal review process, CMS will support state efforts to test incentives that make participation in work or other community engagement a requirement for continued Medicaid eligibility or coverage for certain adult Medicaid beneficiaries in demonstration projects authorized under section 1115 of the Social Security Act.”
The suit challenging Arkansas’ work requirement has been assigned to U.S. District Judge James Boasberg, the same judge who blocked Kentucky’s work requirement. Boasberg on Sept. 12 denied a request by President Donald Trump’s administration and state officials to have the case assigned to a different judge.
Implementation In Arkansas
Beginning June 1, nearly 26,000 Arkansans aged 30-49 who were enrolled in the state’s unique premium-assistance approach to Medicaid expansion — under which the state uses Medicaid funding to purchase individual coverage from qualified health plans through the Health Insurance Marketplace for low-income individuals — became subject to the work requirement and must make monthly reports through an online portal to demonstrate their compliance. Some enrollees can qualify for an exemption, such as those that stay home with a dependent child. Enrollees can satisfy the requirement by showing they spent at least 80 hours of the previous month on work or a combination of other approved activities such as job training or community service.
The work requirement is being phased in this year for Arkansans aged 30-49 and will expand to apply to 19- to 29-year-olds in 2019. The requirement applied to 25,815 people in June and had expanded to apply to 60,012 people by August. Eventually, it will apply to about 167,000 of the 265,000 people enrolled in Arkansas’ Medicaid expansion program. Although the program provides private health insurance to individuals earning up to 138 percent of the federal poverty level, the work requirement applies only to those at or below the federal poverty level.
Enrollees who fail to comply with the requirement for three months during a year are locked out of coverage and cannot apply again until November 1 for coverage starting the following January.
Other States Seeking Work Requirements
New Hampshire’s request for a Medicaid work requirement was approved on May 7; both New Hampshire and Indiana are scheduled to implement their requirements next year. In both states, a person who fails to comply will be able to regain coverage by coming into compliance and will not be locked out for the remainder of the year.
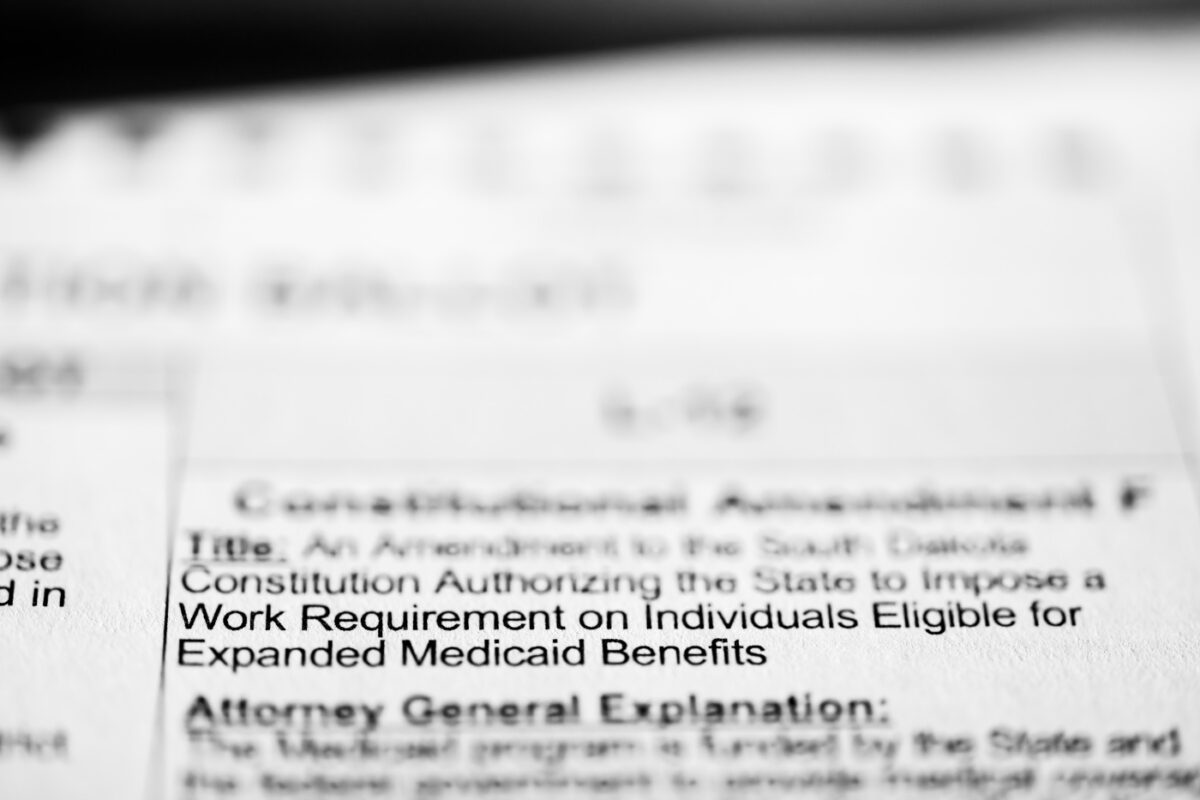
Arizona, Kansas, Maine, Mississippi, North Carolina, Ohio, Utah and Wisconsin have submitted requests for Medicaid work requirements that are awaiting approval. In some states, work requirements are seen as a critical element in winning or maintaining support from conservative legislators for Medicaid expansion. Indeed, Michigan’s legislature and governor have approved a measure that will terminate Medicaid expansion coverage entirely absent federal approval of a work requirement.
Need For Evaluation
At this point, little is known about why thousands of Arkansans failed to comply with the work requirement in its first three months. Some may have failed to comply because they moved out of the state or obtained other coverage. Others may have met the requirement but failed to navigate the online-only reporting system. Arkansas ranks 46th in the nation in internet access and the online system is only available from 7am to 9pm. In a recent Health Affairs Blog post, Jessica Greene, professor and Luciano chair of Health Care Policy at Baruch College, City University of New York, reported that in mid-August she interviewed 18 adult Medicaid recipients in three Northeast Arkansas counties and found “a profound lack of awareness about the policy” despite the state’s efforts to publicize it.
A Section 1115 waiver is by definition an experimental waiver. Section 1115 of the Social Security Act allows the HHS secretary to approve innovations that are likely to assist in promoting the objectives of Medicaid, with the goal of gaining knowledge from state-led experiments that can promote continual improvement of the Medicaid program. Scientifically rigorous evaluation is critical to determine the results of Section 1115 waivers.
Inconsistent Evaluation Messages
However, the Trump administration has at times shown a willingness to loosen the reins on states. In March 2017, then-HHS Secretary Tom Price and CMS Administrator Seema Verma said in a letter to the nation’s governors that they intended to give states more freedom to develop waiver projects and would “fast-track” the federal approval process. In a February report, the Government Accountability Office criticized CMS for not ensuring that states’ Medicaid innovations are evaluated with sufficient rigor. Two months later, the Trump administration granted approval to CMS to scale back plans for the evaluation of Indiana’s Medicaid waiver.
In another twist, on September 12, Verma wrote via Twitter: “I’m excited by the partnerships that Arkansas has fostered to connect Medicaid beneficiaries to work and educational opportunities, and I look forward to our continued collaboration as we thoroughly evaluate the results of their innovative reforms.”
In approving Arkansas’ work requirement, CMS set the terms and conditions for a rigorous scientific evaluation: “The demonstration evaluation will meet the prevailing standards of scientific and academic rigor, as appropriate and feasible for each aspect of the evaluation, including standards for the evaluation design, conduct, and interpretation and reporting of findings. The demonstration evaluation will use the best available data; use controls and adjustments for and reporting of the limitations of data and their effects on results; and discuss the generalizability of results.” The first three years of Arkansas’ waiver for its Medicaid expansion program was subject to an evaluation of the use of premium assistance and commercial coverage for the expansion population meeting these requirements.
Moving Forward
The hypothesis that work requirements lead to enhanced socioeconomic status, maintenance of health insurance coverage and improved health must be assessed and compared to the alternative outcome that needy individuals lose health coverage. A work requirement that leads to a greater number of uninsured people would be an unsuccessful policy; a successful work requirement should guide people into more stable, higher-paying employment and into private health care coverage outside of the Medicaid program.
With a number of states requesting similar waivers to establish work requirements, and with coverage terminations expected to continue in Arkansas each month as long as its waiver stands, the evaluation of this policy should be rigorous, including both routine monitoring and a more in-depth, long-term appraisal. If the courts uphold the administration’s flexibility to establish new Medicaid eligibility requirements, concurrent requirements on the administration to independently evaluate this experimental policy should be strengthened, not loosened.