Author
Michael Motley, MPH
Director, Analytics
Partners
Arkansas Blue Cross and Blue Shield
Arkansas Medicaid
CMS
CHI St. Vincent Hospital
Contact
ACHI Communications
501-526-2244
jlyon@achi.net
Arkansas is a trailblazer in episode-based payment models designed to improve patient outcomes for things like total joint replacements. Our case study details how CHI St. Vincent’s success in Arkansas’s model helped them prepare for similar national programs.
Key Takeaways
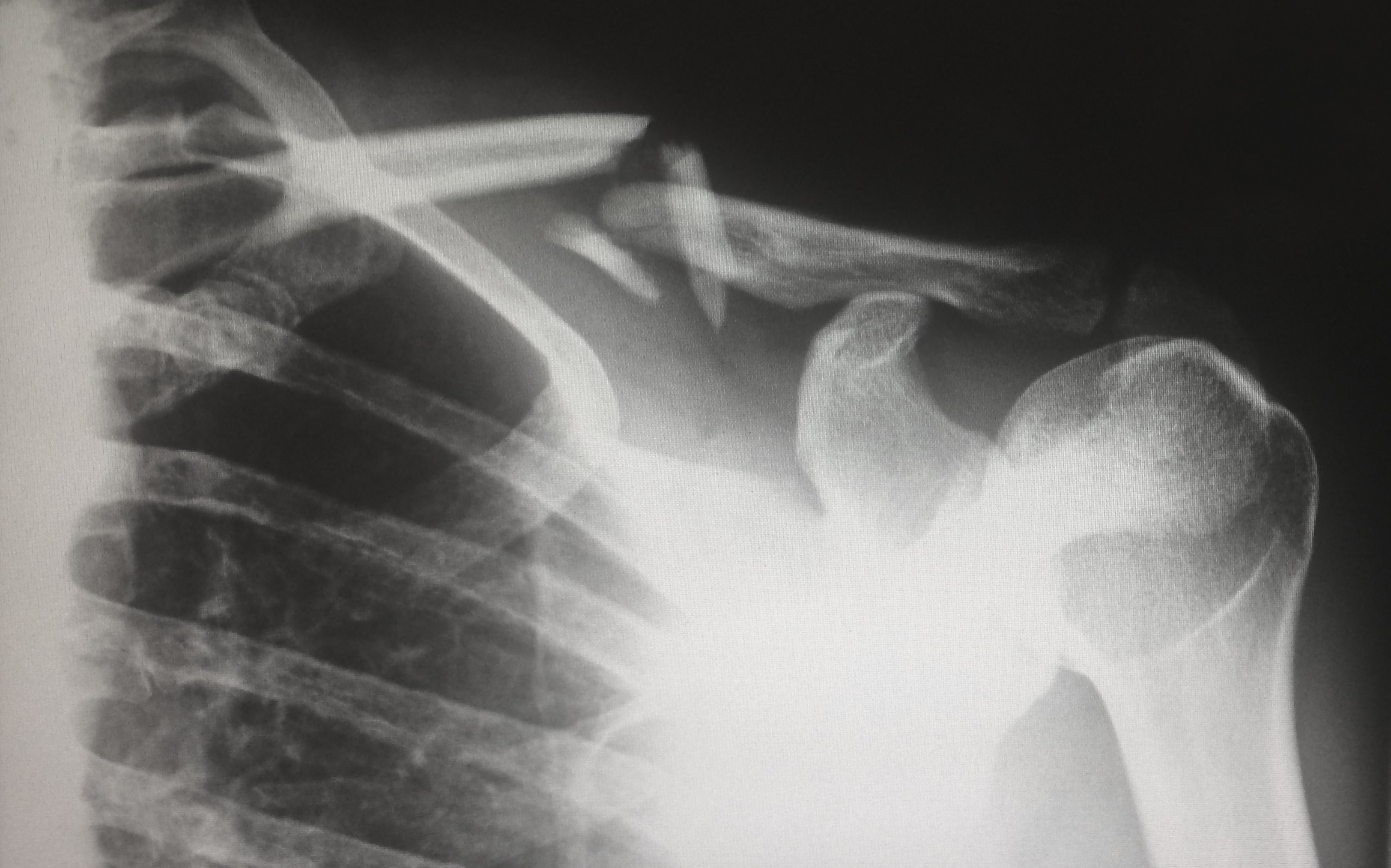
To support high quality care, improve outcomes, and control cost growth, payers have developed alternative payment models for procedures like joint replacements. As a national leader in alternative payment model development, Arkansas launched a unique hip and knee replacement episode in 2013. Later that year, Medicare launched the Bundled Payment for Care Improvement (BPCI) initiative, and in 2016 launched the Comprehensive Care Initiative for Joint Replacement (CJR). A new BPCI Advanced model will be launched in 2018.
Launched in 2012, Arkansas’s Episodes of Care model is designed for conditions that require care coordination and intensive use of resources. In an Episode of Care (EOC), payers identify a principal accountable provider (PAP) to manage the quality and minimize treatment variations. Through identified opportunities to improve quality and reduce complications for the entire episode, pre-established performance expectations enable PAPs to benefit from system efficiencies. Quarterly reports detail individual performance metrics for each PAP. Providers are eligible to share in any savings that occur if they achieve quality targets. PAPs with average costs above an acceptable threshold are subject to share risks and excess costs.