Arkansas Healthcare Workforce
This page serves as a resource for ongoing analysis to provide insight into healthcare workforce challenges and opportunities.
Primary Care Physician Workforce Dashboard
The Journey To Become a Physician in Arkansas
Reports and Explainers
News and Updates
Arkansas, like other states, faces a shortage of physicians, nurses, and other healthcare providers. Provider shortages continue to be one of the most pressing challenges faced by healthcare organizations and communities seeking to ensure access to quality care for their residents. The challenge is compounded by geographic maldistribution, with more than one-third of Arkansans living in health professional shortage areas. In 2020, six of the state’s counties had only one full-time primary care physician.
Primary care physician shortages in particular have been associated with higher rates of preventable emergency department visits. Conversely, greater primary care physician supply has been associated with earlier diagnosis of disease, lower mortality, and lower costs.
The state has made considerable progress in developing the health workforce pipeline following a statewide strategic planning effort, but addressing the challenge requires a significant, growing commitment to ensure a stronger, larger, more coordinated, and robust health workforce that can meet the state’s future health and healthcare needs.
PROFILE OF THE PRIMARY CARE PHYSICIAN WORKFORCE IN ARKANSAS
ACHI has developed an interactive dashboard to examine the primary care physician workforce in Arkansas. With data for calendar years 2019 through 2022, the dashboard provides visualizations at the state, county, and regional levels and includes information on physician demographics and activity status (full-time, part-time), payer mix, and primary care subspecialties such as family medicine, internal medicine, general practice, pediatrics, and geriatrics.
The dashboard is intended to inform policymakers, healthcare leaders, and other stakeholders about the supply, characteristics, and distribution of PCPs so they can make evidence-based decisions regarding provider access across Arkansas communities.
The data presented in this dashboard were obtained from the Arkansas Healthcare Transparency Initiative’s All-Payer Claims Database, licensure files from the Arkansas State Medical Board, and CarePrecise. Key findings based on 2022 data include:
- There were 2,791 active primary care physicians in Arkansas in 2022, or 9.3 per 10,000 residents.
- About 38% of PCPs practiced fewer than 150 active days during the year.
- 26% of full-time PCPs were age 60 or older, raising concerns about future supply as many approach retirement.
- Early-career PCPs (under age 45) were more likely to practice fewer than 150 days during the year compared to PCPs age 45 and up (41% vs 35%).
- The PCP workforce continued to show differences by sex: 67% were male and 33% were female, although differences narrowed among younger physicians.
- Racial and ethnic diversity remained limited: While Black and Hispanic Arkansans made up 14.9% and 8.8%, respectively, of the state’s population, they represented only 6% and 3%, respectively, of active PCPs.
This work is made possible with funding from the federal Health Resources and Services Administration (HRSA) and support from the University of Arkansas for Medical Sciences.
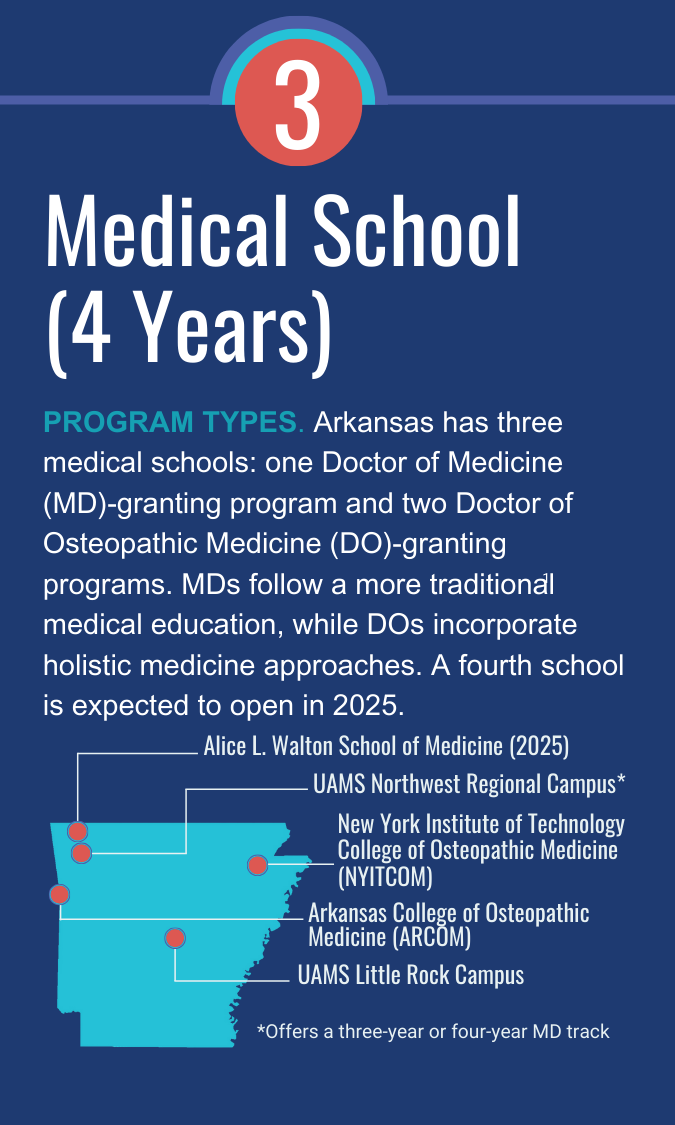
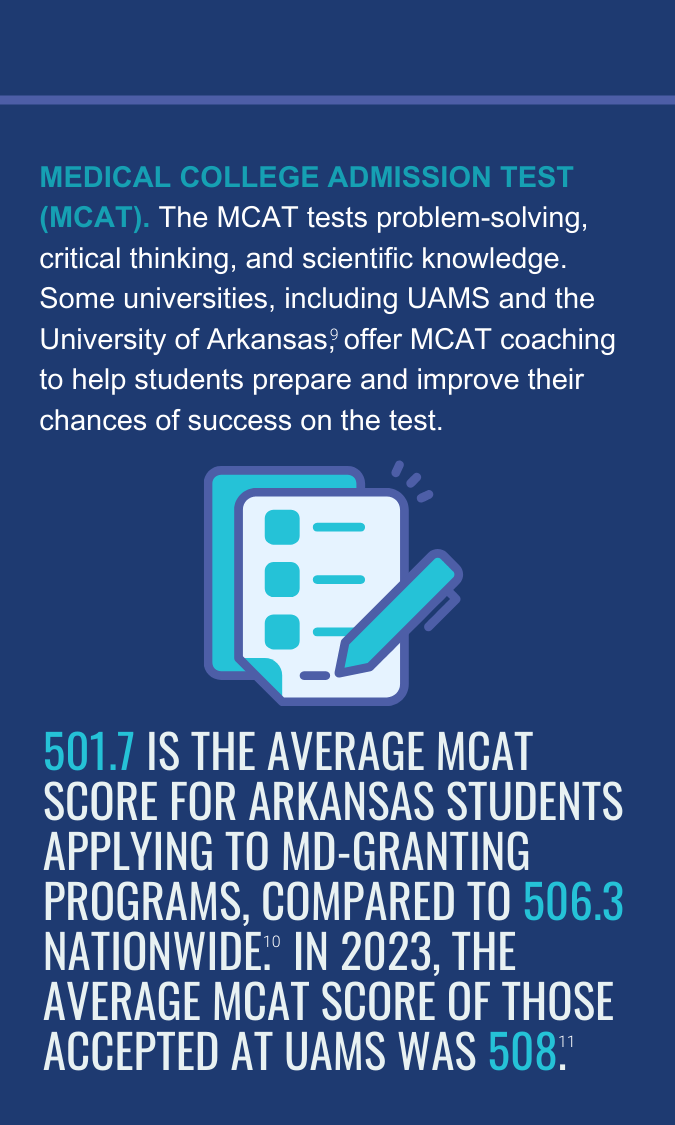
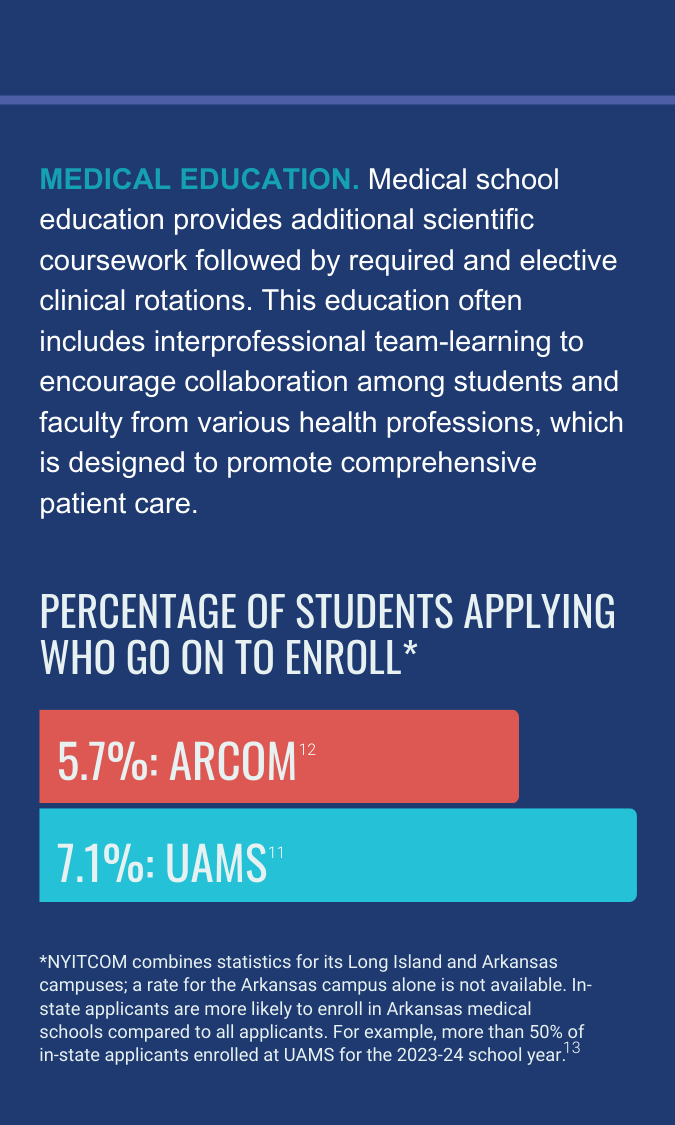
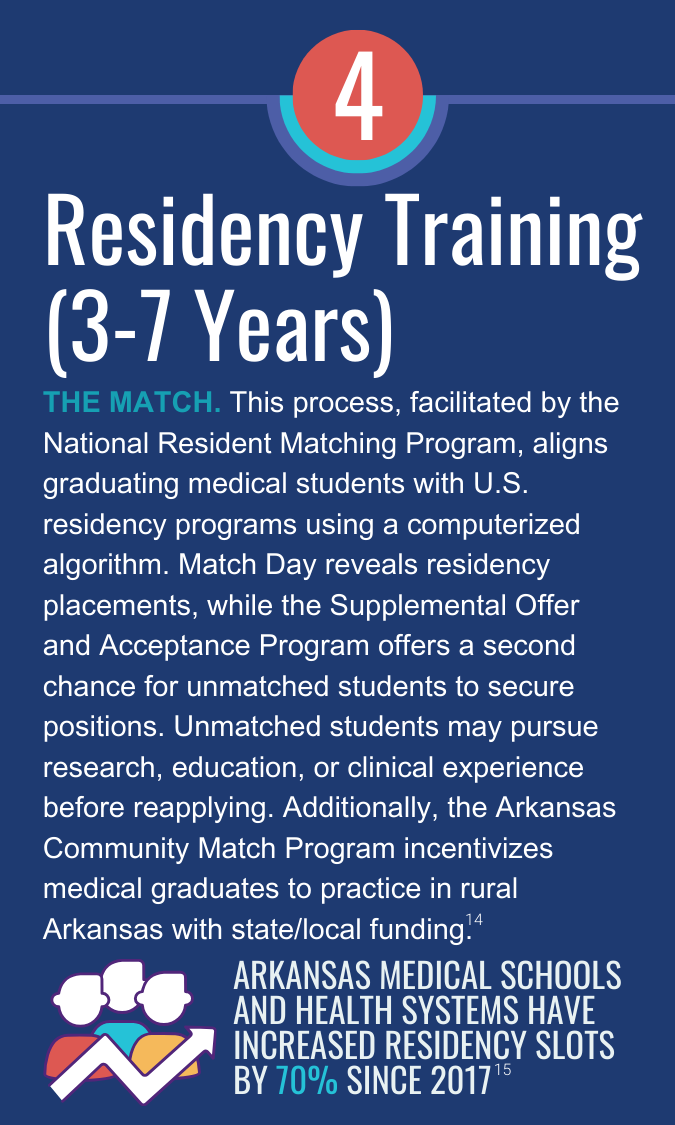
The journey to become a physician in arkansas
As of 2020, the state ranked among the lowest in the nation in terms of per capita physician workforce. Arkansas needs to expand its physician workforce pipeline — but these healthcare providers are not created overnight.
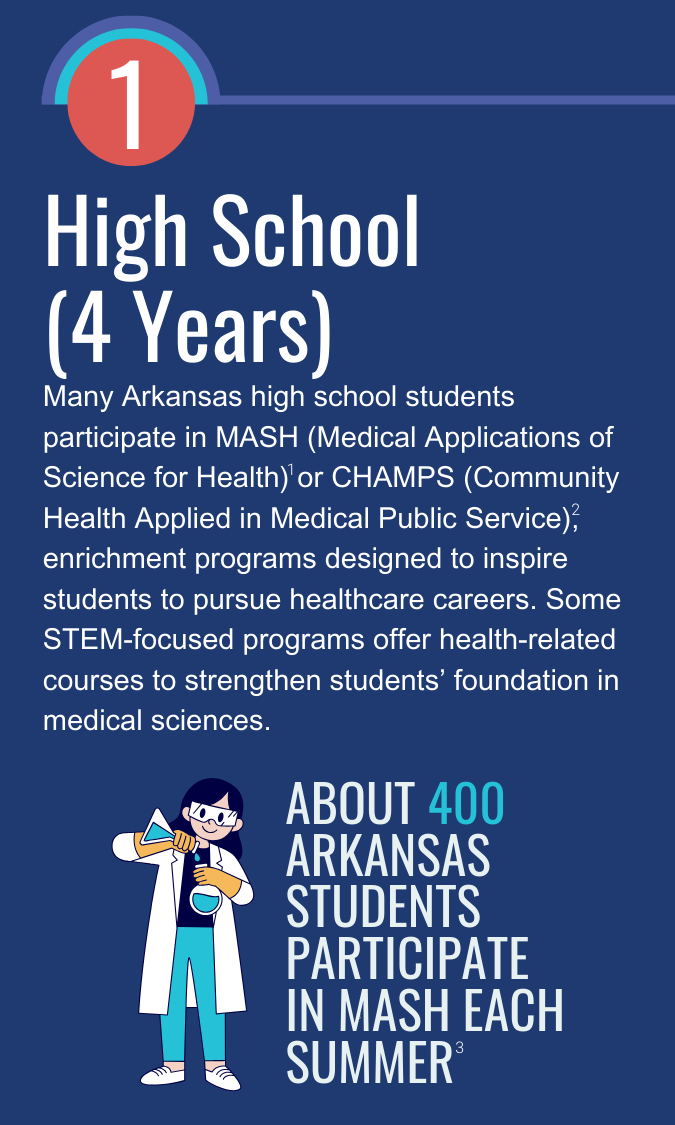
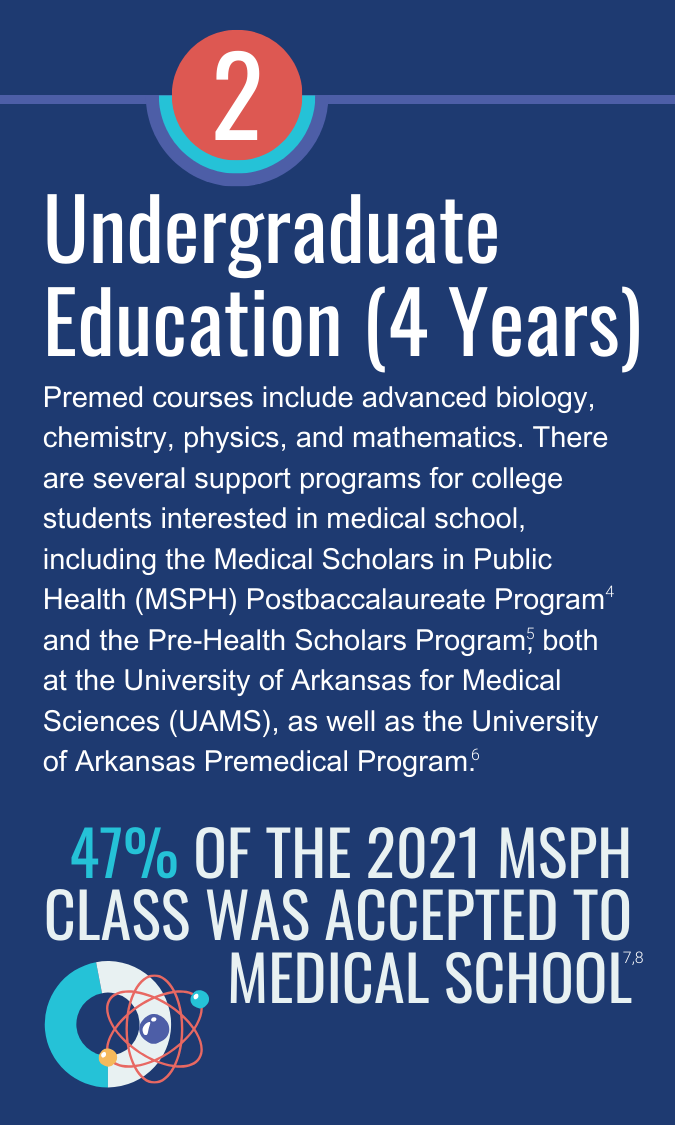
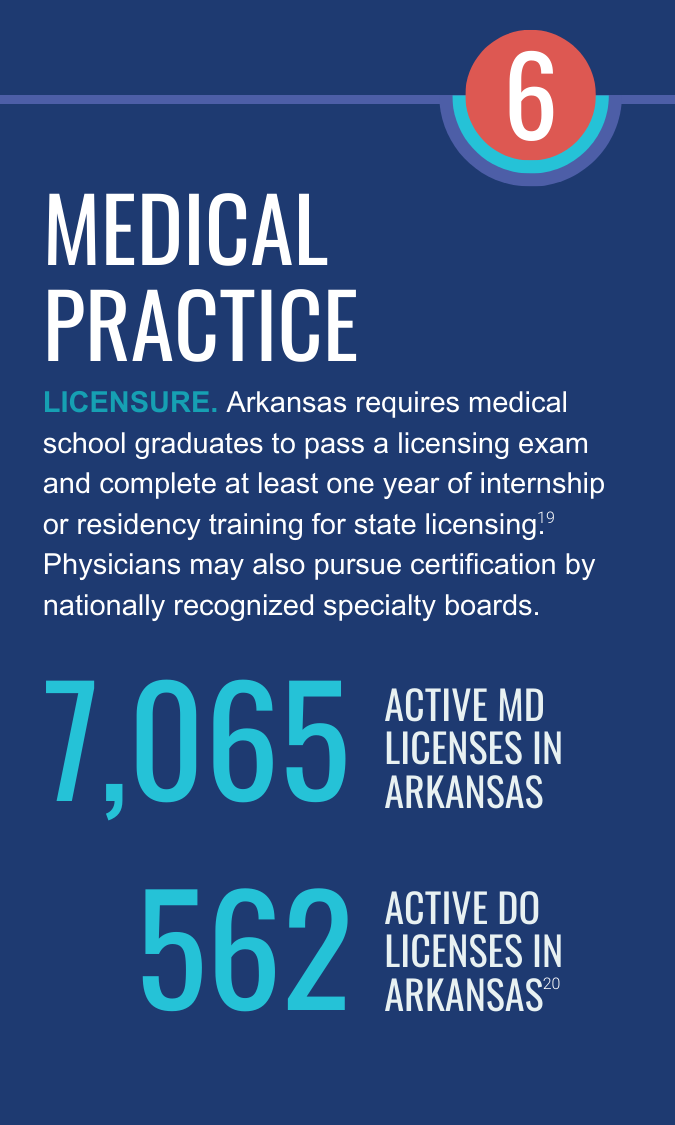
This infographic outlines the multi-step journey to become a physician in Arkansas, emphasizing the extensive education and training required.

Related Reports and Explainers
Learning To Fly: Robin Howell
Cultivating interest in healthcare careers among students earlier in the educational process is key to ensuring a sufficient workforce pipeline to respond to the needs of Arkansans. That has been the focus of Robin Howell, senior program manager for regional campuses at the University of Arkansas for Medical Sciences, for more than 35 years. In this episode, host Craig Wilson talks with Howell about the Medical Applications of Science for Health (MASH) program, a summer enrichment camp that allows high school students to learn about health career opportunities, and other efforts to develop a strong physician workforce pipeline in Arkansas. August 10, 2023.