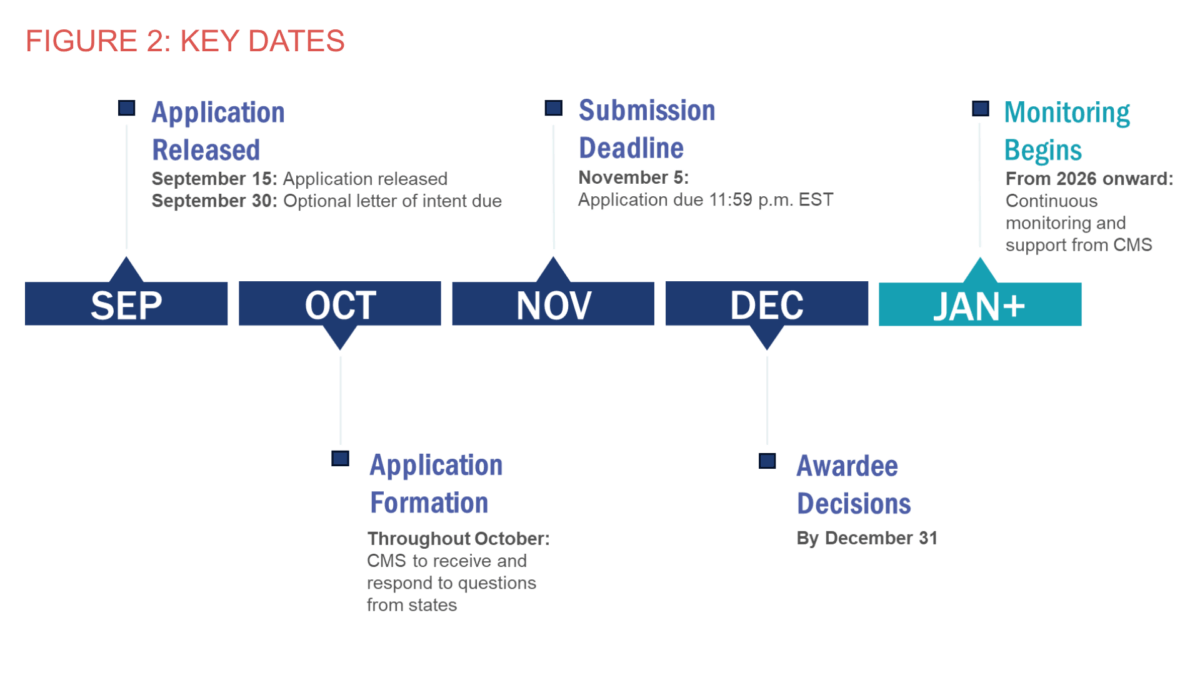
On July 4, 2025, President Donald Trump signed H.R. 1, enacting sweeping changes to federal spending and tax policy. The law’s provisions affecting spending on Medicare, Medicaid, and other healthcare coverage programs will disproportionately affect rural health systems that rely heavily on public insurance programs. Recognizing this, Congress included a “Rural Health Transformation Program” in the final bill — a $50 billion fund allotted to the states over five years — to soften the impact of funding reductions on rural communities. States must apply for funds by November 5, 2025;1 approval of an application is valid for the full five-year period.
Because of its large populations of rural and low-income residents, many of whom rely on public healthcare coverage programs, Arkansas will be differentially impacted by changes in the federal law. About 45% of Arkansans live in rural areas, where residents face less access to health care, worse healthcare outcomes, and more fragile healthcare systems than residents of urban areas.2 Although Arkansas has been spared when it comes to hospital closures compared to surrounding states over the last decade, 50% of rural hospitals in Arkansas are currently vulnerable to closure — the highest percentage in the nation.3 Given these risks, it is critical that Arkansas’s Rural Health Transformation funds be spent on promoting the long-term financial stability of rural healthcare providers. The program offers an opportunity to build efficient, collaborative, and sustainable rural healthcare infrastructure and reduce the rural-urban gap in healthcare access and quality of care.
It is difficult to estimate how much Arkansas will receive under the program based on the legislation and current guidance from the Centers for Medicare and Medicaid Services (CMS), but it is anticipated that the $50 billion fund will not be enough to offset the loss of revenue from other sources that rural areas of the country will experience.4 More broadly, the law represents a clear shift in responsibility for fiscal support of health care from the federal government to the states and local communities. In this context, it is critical that rural leaders understand the health needs of their communities and their capacity to collaborate regionally to ensure resources are used effectively.
An October 1 news release from Gov. Sarah Huckabee Sanders’ office announced the state’s intention to apply for the program and announced the creation of an online portal through which interested stakeholders could submit proposals for inclusion in the state’s application to CMS.5 Sanders’ office said the state would accept proposals through October 10, after which submissions would be accepted but were not guaranteed to be reviewed.
Table of Contents
Program Details
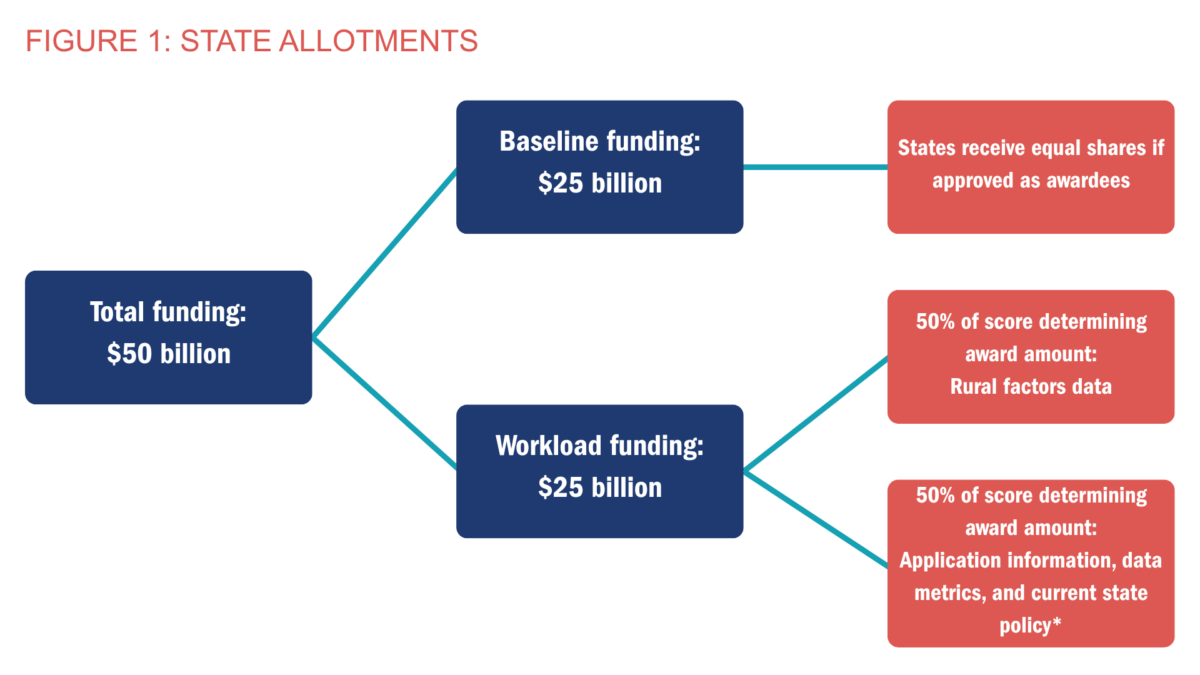
The Rural Health Transformation Program allocates $50 billion over five years to be distributed to the 50 states (Washington, D.C., and the U.S. territories are not eligible) and spent on specific rural healthcare activities.
STATE ALLOTMENTS
“Rural health facilities” are defined in the legislation as (paraphrased):
- Any hospital that is in a rural area by CMS determination or is in a rural census tract of a metropolitan statistical area (MSA)
- Critical access hospitals
- Sole community hospitals
- Medicare-dependent, small rural hospitals
- Low-volume hospitals
- Rural emergency hospitals
- Rural health clinics
- Federally qualified health centers
- Community mental health centers
- Any health center receiving a grant under Section 330 of the Public Health Service Act
- Any opioid treatment program in a rural census tract of an MSA
- Any certified community behavioral health clinic in a rural census tract of an MSA
The money will be allotted to states in two tranches:
- $25 billion of “baseline funding” will be allotted evenly among all states with approved applications, without respect to each state’s total or rural population, number of rural health facilities, or need demonstrated in the application.
- Assuming all 50 states apply and are approved, Arkansas would receive $100 million annually, as would all other states.
- CMS is not required to approve all states that apply. If any states either do not apply or have their applications denied, the annual allotment to each approved state through the first tranche would be more than $100 million.
- $25 billion will be allotted as “workload funding,” determined through a points-based scoring system. The scoring will incorporate two sets of factors:6
- Rural population and facility factors, including rural population size, proportion of facilities located in rural census tracts, uncompensated care, share of population living in rural tracts, frontier and land-area metrics, and disproportionate share hospital status.
- Technical factors, including state workforce recruitment and retention strategies, participation in licensure compacts, Medicaid provider payment incentives, scope-of-practice restrictions, remote care services, and health data infrastructure.
There is no guarantee that approved states will receive the second tranche of funds. However, CMS is required to make allotments to at least a quarter of approved states.4
Adapted from Rural Health Transformation Program: Opportunity Number: CMS-RHT-26-001, Centers for Medicare and Medicaid Services, available from https://www.grants.gov/search-results-detail/360442
*This portion of workload funding is recalculated annually to reflect progress made by each state on technical factors identified in its application.
ALLOWABLE COSTS
States will have broad discretion in spending the funds, but the legislation lists 10 explicitly allowable costs and activities (paraphrased):a
- Payments to healthcare providers.
- Uses promoting evidence-based interventions for prevention and management of chronic disease.
- Uses promoting of technology-driven solutions for prevention and management of chronic disease.
- Training and technical assistance for technology-enabled solutions to improve care in total hospitals, such as robotics, AI, and remote monitoring.
- Recruitment and retention of clinical workforce talent to serve rural areas, with a minimum five-year commitment.
- Technical assistance, software, and hardware for information technology advances improving efficiency, cybersecurity, and patient outcomes.
- Right-sizing of rural healthcare delivery systems through identification of needed service lines.
- Uses supporting access to opioid use disorder treatment, other substance use disorder treatment, and mental health services.
- Uses supporting innovative care models, including value-based care arrangements and alternative payment models.
- Additional uses promoting sustainable access to rural healthcare services, as determined by the CMS administrator.
States must spend their allotments on at least three of the above. A maximum of 10% of a state’s allotment may be for administrative purposes. States have no matching requirement for Rural Health Transformation Program funds.
Additional restrictions apply. Funds may not be used for construction, building expansion, or cosmetic renovations that increase the “value of the capital or useful life” (although limited renovations and alterations are allowable with up to 20% of a state’s allotment). Funds also may not be used for lobbying, supplanting existing federal or state funding, transferring expenditures between different levels of government, or financing the non-federal share of other programs.4
APPLICATION FOR FUNDING
To receive an allotment, a state must submit an application responsive to funding opportunity CMS-RHT-26-001.6 The application must be paired with a written endorsement from the state’s governor. The legislation specifies that the application must contain (paraphrased):
- A “Rural Health Transformation Plan” that:
- Improves access to healthcare items and services for rural residents.
- Improves healthcare outcomes of rural residents.
- Prioritizes the use of emerging technologies for prevention and management of chronic disease.
- Initiates and strengthens strategic partnerships between rural hospitals and other providers to promote quality improvement and financial stability, maximize economies of scale, and share best practices.
- Enhances economic opportunity for, and the supply of, clinicians through enhanced recruitment and training.
- Prioritizes data and technology-driven solutions to furnish healthcare service as close to patients’ homes as possible.
- Outlines strategies for managing long-term financial solvency and operating models for rural hospitals.
- Identifies specific causes for the increasing rate of stand-alone rural hospital closure, conversion, or service reduction.
- A certification that funds shall not be used for expenditures attributable to an intergovernmental transfer, certified public health expenditures, or expenditures financing the non-federal share of other programs required under any provision of law.
- “Such other information as the administrator may require.”
A September 15 funding announcement from CMS lists specific program priorities for applications to target and describes the points system used to assess each state plan’s responsiveness to these priorities.1
Adapted from Rural Health Transformation (RHT) Program, Center for Medicare and Medicaid Services, https://www.cms.gov/priorities/rural-health-transformation-rht-program/rural-health-transformation-rht-program
Approval of the initial application qualifies a state for the full five years of funding; there is no requirement for annual reapplication.
The legislation requires each state receiving funds to submit annual reports on how the funds are used, “including such additional information as the administrator determines appropriate.”
Lessons From the American Rescue Plan Act
The American Rescue Plan Act (ARPA) of 2021 provided a $2.6 billion stimulus to the state of Arkansas, split between state, county, and local governments. Similarly to the Rural Health Transformation Program, ARPA gave broad freedom to recipients to direct funds where they saw fit, within certain guidelines — funds could be used to support the COVID-19 response, fill revenue shortfalls, and address the disparate impact of the pandemic on various populations.
While ARPA was a critical lifeline for communities across the nation, urgency to spend and minimal guidance on priorities led to much of the money being used on short-term relief rather than long-term strengthening of health systems. The Rural Health Transformation Program is similar in that regard. It could be used to fill gaps in funding and provide short-term direct support to healthcare providers — which will be needed — but it could also be used to make strategic investments that promote long-term financial stability and improve quality and continuity of care in rural healthcare systems.
Funding Considerations
The Rural Health Association of Arkansas has adopted a set of recommendations for dispensing the state’s allocation of rural transformation funds. The association’s recommendations suggest a framework for vetting proposals from entities seeking to fund initiatives, services, and other assistance and recognize the heightened need for data-driven decision-making, technological innovation, collaboration, and community engagement. The recommendations are:
DEVELOP A FAIR AND TRANSPARENT PROCESS FOR DISPENSING AND MONITORING FUNDS
- Establish clear goals and criteria for applicants.
- Conduct open meetings for application consideration and publicly report spending in a detailed and transparent manner.
- Ensure heightened scrutiny of applications which include partners, vendors, or investors that might create conflicts of interest or unintended consequences for healthcare quality and access. Require disclosure of financial status, risks, and relationships.
- Make funding contingent on explicit service delivery commitments and ensure that funds are used either directly or indirectly for the benefit of rural health in Arkansas.
EMBRACE A REGIONAL MINDSET
- Recognize the interdependence of rural communities and the potential benefits of regional approaches to service delivery, including collaboration across sectors when appropriate.
- Encourage applications that pool resources and expertise and demonstrate long-term, formal regional networks for prevention, treatment, rehabilitation, and other efforts, with capacity to share services and reduce travel burdens for patients.
- Use state oversight to remove collaboration barriers and leverage resources.
- Support non-traditional sites of service and explore innovative partnerships and technology that expand regional reach.
USE EVIDENCE TO GUIDE FUNDING DECISIONS
- Prioritize funding of initiatives that are supported by evidence.
- Assess specific needs and demand for services within rural populations, including outmigration of services that could be provided locally, with a focus on mitigating negative impacts on access and ensuring support for those with the greatest health needs.
- Monitor fiscal impacts of federal and state policy on rural healthcare providers and direct funding correspondingly.
SUPPORT ESSENTIAL SERVICES WHILE ENCOURAGING INNOVATION
- Safeguard emergency services through payments for fixed costs so that providers offering those services can absorb standby capacity, even when patient volume and related revenue are not high enough to cover the expenditures.
- Encourage demonstration initiatives that are accompanied by scientifically rigorous evaluations.
- Reduce financial barriers to invest in shared technology for remote delivery of care and patient data exchange.
- Strengthen local access to primary care including preventive care and chronic disease management, maternal care, and the ability to identify and address health-related social needs.
- Bolster transportation for follow-up services that directly support patient access to services not locally available.
INVEST NOT ONLY IN INFRASTRUCTURE AND INSTITUTIONS BUT ALSO IN PEOPLE
- Identify facility or equipment challenges that serve as a barrier to optimizing service delivery.
- Invest in technical assistance to support adoption of technology-enabled solutions; financial stewardship; workforce recruitment, retention, and training; and administrative or governance capacity.
- Engage community members in identifying and prioritizing their most pressing needs and ensure that community-based mental health services are part of the conversation.
While the rural transformation funds are not expected to fully mitigate the revenue impact from coverage loss and other federal policy changes, Arkansas has an opportunity to pursue targeted investments leading toward sustainability. Maintaining the status quo of Arkansas’s healthcare system is not an option, particularly given the state’s changing population dynamics, shifts in technology and payment models, and increasing specialization of care. Supporting the creation of collaborative healthcare systems such as shared service models, consolidated billing services, and joint contracting would facilitate the development of economies of scale among networks of small rural facilities. Ensuring sufficient Medicaid payment for and assisting eligible and interested facilities in converting to rural emergency hospital (REH) status should be explored. In addition, several options exist to target statewide needs, including developing a statewide closed-loop referral system to address social needs; establishing a hospital board education program; developing programs offering grant writing support and technical assistance for revenue management, staffing, and professional development to rural providers; and facilitating the standardization and modernization of healthcare professional licensure data collection, which could provide cross-profession data to guide planning and policy decisions.7 These investments could greatly improve the quality, efficiency, and sustainability of rural health care throughout the state.
Conclusion
The Rural Health Transformation Program presents an opportunity to invest in promoting an innovative and sustainable healthcare system in rural Arkansas. While uncertainty remains as to the size of Arkansas’s allotment through the program, annual payments in the hundreds of millions should be expected starting in 2026. With timely and deliberate implementation, the program has the potential to both soften the short-term impact of federal funding cuts and improve the long-term financial viability of Arkansas’s rural healthcare providers.
References
1 Centers for Medicare and Medicaid Services. CMS launches landmark $50 billion Rural Health Transformation Program. CMS.gov. September 15, 2025. Accessed September 25, 2025. https://www.cms.gov/newsroom/press-releases/cms-launches-landmark-50-billion-rural-health-transformation-program
2 University of Arkansas System, Division of Agriculture, Cooperative Extension Service. 2025 Rural Profile of Arkansas. 2025. Accessed October 1, 2025. https://www.uaex.uada.edu/publications/pdf/MP585.pdf
3 Chartis. 2025 Rural Health State of the State. 2025. Accessed October 1, 2025. https://www.chartis.com/sites/default/files/documents/CCRH%20WP%20-%202025%20Rural%20health%20state%20of%20the%20state_021125.pdf
4 Levinson Z, Neuman T. A closer look at the $50 billion Rural Health Fund in the new reconciliation law. KFF. August 4, 2025. Accessed August 7, 2025. https://www.kff.org/medicaid/issue-brief/a-closer-look-at-the-50-billion-rural-health-fund-in-the-new-reconciliation-law/
5 Sanders announces portal for Rural Health Transformation Program proposals. Office of Arkansas Governor Sarah Huckabee Sanders. October 1, 2025. Accessed October 2, 2025. https://governor.arkansas.gov/news_post/sanders-announces-portal-for-rural-health-transformation-program-proposals/
6 Centers for Medicare and Medicaid Services. Rural Health Transformation Program: Opportunity Number: CMS-RHT-26-001. Accessed September 17, 2025. Available at: https://www.grants.gov/search-results-detail/360442
7 Maxey H, Medlock C. Why we can’t count our doctors (and how to fix it). Health Affairs. September 16, 2025. Accessed September 25, 2025. doi:10.1377/forefront.20250915.475022
a Note that not all of the allowable costs explicitly require that spending be directed toward rural areas or rural health facilities. This means that, depending on the purpose of the spending, some funds may be directed toward urban and suburban facilities. The second tranche’s points system rewards applicants for spending on rural facilities in some cases where rural spending is not required.