Author
John Lyon
Strategic Communications Manager
Contact
ACHI Communications
501-526-2244
jlyon@achi.net
Rural Americans face significant challenges in accessing primary care, but there are opportunities for policymakers and healthcare leaders to address these issues, according to a new issue brief from The Commonwealth Fund. In “The State of Rural Primary Care in the United States,” the organization assesses the issues facing rural primary care, highlights communities that have implemented innovative solutions, and identifies policy options.
National Challenges
Drawing on the Commonwealth Fund 2023 International Health Policy Survey and federal health workforce data, the brief finds that:
- In 2023, the supply of primary care physicians met only about 69% of the demand in rural areas — a figure that isn’t projected to change much over the next several years.
- In 2023, 92% of rural counites in the U.S. were designated by the Health Resources and Services Administration as health professional shortage areas (HPSAs), although there were regional disparities. In the South and West, 97% of rural counties were designated partially or wholly as HPSAs, compared to 84% in the Midwest.
- 43 million people lived in rural areas with primary care health professional shortages in 2023.
- About 1 in 5 rural adults (19%) reported in 2023 that they had received primary care via telehealth in the past 12 months, compared to the national average of 29%.
Innovative Solutions
The brief notes that despite these challenges, many rural communities have implemented innovative solutions to their healthcare access problems. It highlights two programs:
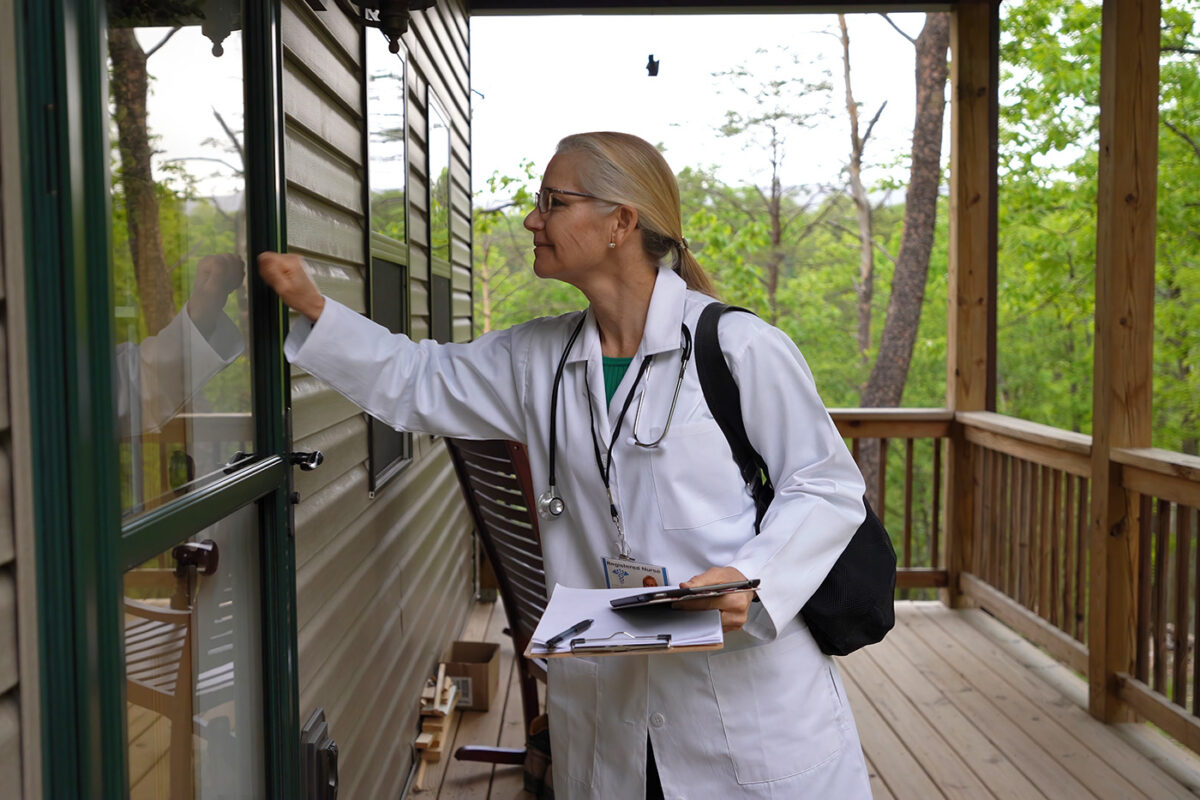
- Kentucky Homeplace, developed by the University of Kentucky Center for Excellence in Rural Health, leverages community health workers to address that state’s primary care physician shortage. Community health workers live in the local community and create a bridge between residents and the healthcare, public health, and social service systems. Between 2001 and 2024, Kentucky Homeplace served over 196,000 patients and provided over 5 million services.
- The Physician Shortage Area Program, developed by the Sidney Kimmel Medical College at Thomas Jefferson University in Pennsylvania, selectively admits medical school applicants from rural areas who are committed to practicing rural primary care in the future. The program has trained more than 300 physicians since 1974, accounting for 21% of all rural physicians in Pennsylvania. Evaluations of the program have found that 70% of participants stay in rural areas for 20 to 25 years, and 10% have moved to other rural areas.
Policy Options
The Commonwealth Fund suggests the following policy options for strengthening rural primary care:
- Design rural-specific financing options. Payment reform such as enhanced reimbursements, bonus payments, upfront infrastructure investments, and payments tied to operational costs could mitigate the lack of funding in rural care delivery. For example, the Pennsylvania Rural Health Model provides consistent payments not tied to patient volume.
- Grow the pipeline of healthcare clinicians. Healthcare system and policy leaders can grow the rural workforce pipeline by targeting local recruitment of healthcare workers, incorporating rural rotations into medical school training, increasing opportunities for rural residencies and experiential learning, and incentivizing medical practice in rural areas through loan repayment programs.
- Strengthen rural technology infrastructure. Policymakers can invest in broadband infrastructure and promote payment parity and training for telehealth and other digital innovations to ensure clinicians have the capacity and financial means to deliver telehealth services.
Arkansas Challenges
ACHI’s analyses of Arkansas data show that rural Arkansans have limited access to primary care and maternity care compared to their urban counterparts. Our interactive dashboards profiling the state’s primary care physician workforce and its obstetrics and gynecology (OB-GYN) physician workforce show that in 2022:
- The rate of primary care physicians practicing in rural counties was 10.3 physicians per 10,000 residents, compared to 12.6 physicians per 10,000 residents in urban counties.
- 50% of primary care physicians in rural counties practiced less than full time, compared to 43% primary care physicians in urban counties.
- The rate of OB-GYNs practicing in rural counties was 2.9 OB-GYNs per 10,000 residents, compared to 4.3 OB-GYNs per 10,000 residents in urban counties.
- 49% of OB-GYNs in rural counties practiced less than full time, compared to 29% of OB-GYNs in urban counties.
Several recent actions by Arkansas policymakers are aimed at filling gaps in the state’s healthcare system, including in rural areas. Among other things, the Arkansas General Assembly has approved measures to create a working group on primary care payment improvement, join interstate licensure compacts to make it easier for physicians and other healthcare professionals to practice in multiple states, increase the number of medical residency positions in the state, require insurers to cover services provided in mobile health units, offer loan forgiveness to mental health professionals who agree to practice in underserved areas, and establish reimbursement pathways for maternal health services provided by doulas and community health workers.
Arkansas also has applied for funding through the Rural Health Transformation Program, a $50 billion federal investment in rural health care that was included in the 2025 budget reconciliation law. The state’s application proposes four new initiatives comprising 19 programs focused on long-term, systemic improvements to health and health care in rural Arkansas, as we discussed in a previous post.
More information is available on our Rural Health Insights, Maternal and Infant Health, and Arkansas Healthcare Workforce topic pages.