
Author
John Lyon
Strategic Communications Manager
Contact
ACHI Communications
501-526-2244
jlyon@achi.net
Arkansas lawmakers last week began the process of reviewing two proposed rules aimed at improving maternal health outcomes in the state. The state Department of Human Services drafted the rules as part of the implementation of the Healthy Moms, Healthy Babies Act, an omnibus law encompassing key components of Gov. Sarah Huckabee Sanders’ maternal health agenda for 2025. The rules would create presumptive Medicaid eligibility for pregnant women and revamp and increase Medicaid reimbursement for obstetric services.
Presumptive Eligibility
Presumptive eligibility is a policy that allows pregnant women to receive temporary coverage while their Medicaid eligibility application is being processed, thereby removing one barrier to beginning prenatal health care that some women face. At least 28 other states provide presumptive eligibility to pregnant women, according to a 2025 survey.
For the best chance of a healthy pregnancy and delivery, a pregnant woman should begin receiving prenatal care in the first trimester, but in Arkansas, nearly 1 in 10 women who gave birth in 2023 had received no prenatal care or care that began late. Inadequate prenatal care is believed to be one many factors contributing to Arkansas’s poor maternal health outcomes. The state has the fourth-highest maternal mortality rate and the third-highest infant mortality rate in the nation. In a 2024 report, the Arkansas Strategic Committee for Maternal Health included presumptive eligibility among its policy recommendations.
In a joint meeting on June 4, the House and Senate Public Health, Welfare and Labor committees reviewed the proposed rule on presumptive eligibility with no objections. The proposed rule states that a pregnant woman who applies for pregnancy Medicaid will immediately receive coverage for prenatal services and services for conditions that may complicate the pregnancy, based on her self-attestation of income and residency. The services must be provided in an outpatient setting. This temporary coverage generally continues through the end of the month following the month in which eligibility is determined. A fiscal impact statement presented to lawmakers estimates that the rule will cost about $1.6 million in the fiscal year that begins July 1, with the state paying about $487,000 and the federal government paying the rest.
The Department of Human Services will work with healthcare providers and community organizations to educate pregnant woman about the availability of presumptive Medicaid eligibility, Elizabeth Pitman, director of the Division of Medical Services for Arkansas Medicaid, told the committees on June 4.
Reimbursement for Obstetric Services
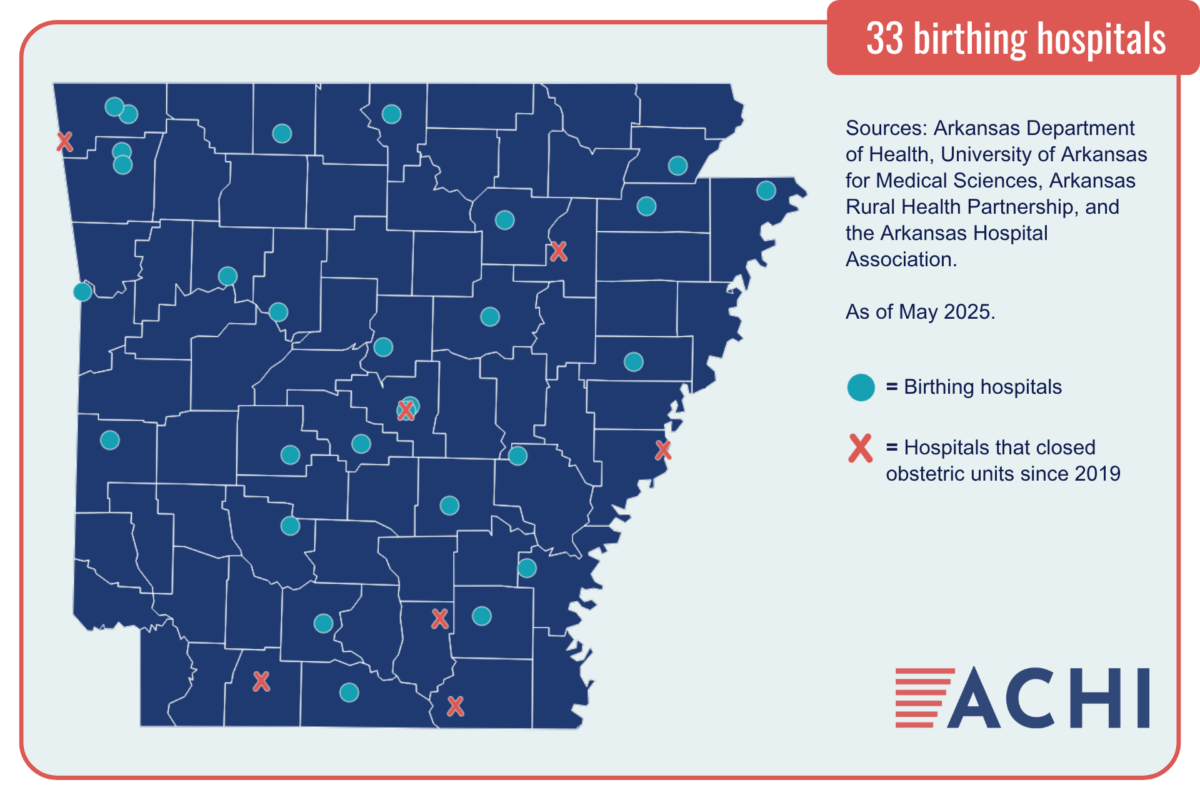
The committees also reviewed without objection a proposed rule that would increase Medicaid reimbursement rates for obstetric services, including prenatal care, labor and delivery services, and postpartum care, by 70%. The increase is intended to improve access to those services in rural areas, which have seen several hospitals close their labor and delivery units in recent years. As of May, Arkansas had 33 birthing hospitals, down from 40 in 2019.
The rule also would require Arkansas Medicaid to reimburse healthcare providers for obstetric services separately rather than in one combined, or “bundled,” payment per delivery. The change is intended to improve the state’s ability to collect data on utilization of prenatal and postpartum services, the committees were told during the June 4 meeting.
The rule is estimated to cost about $38 million in the fiscal year that begins July 1, with the state paying about $12 million and the federal government paying the rest.
Both proposed rules must be reviewed next by the Administrative Rules Subcommittee of the Arkansas Legislative Council and then by the full council before they can be implemented. Since Medicaid is a joint state and federal program, Arkansas also will need to obtain approval for the changes from the federal Centers for Medicare and Medicaid Services. The proposed date for both rules to take effect is July 1.
See more about maternal and infant health in Arkansas on our topic page.






